- Joined
- Aug 14, 2012
- Messages
- 984
- Reaction score
- 9
Why do we get opacification of the involved lung in atelectasis on CXR?



No air and increased tissue density. That's why it's helpful to get an expiratory film when you suspect foreign body aspiration--the side with foreign body will have trapped air and thus be hyperlucent (at least according to Felson's).
This confused me a lot so I had to look it up. Apparently kids more frequently get air trapping (which would present with the hyperlucency you describe) while adults tend to get atelectasis. Atelectasis also often doesn't show up until >24 hr post aspiration
This is why, by the way, 100% O2 can sometimes cause absorption atelectasis--because there's no nitrogenous stent keeping the alveoli open as the O2/CO2 equilibrate.
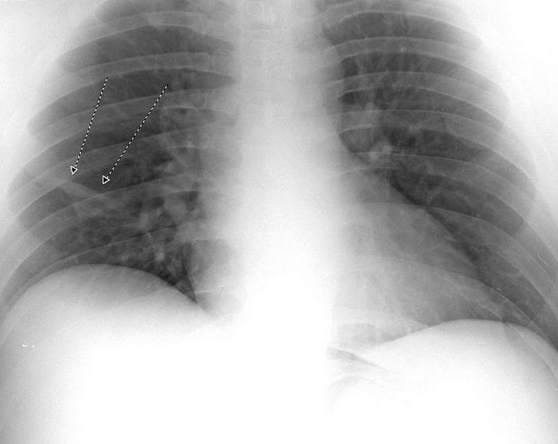
There aren't any signs specific to atelectasis on that CXR, but a hyperdense right side combined with tracheal deviation to the right (indicating volume loss) is well explained by atelectasis
Interesting! Thanks for sharing. Is this a feature of low N2 diffusion rate, high N2 stores in proximal fluids, or something else I'm not thinking of
