- Joined
- May 4, 2016
- Messages
- 54
- Reaction score
- 15
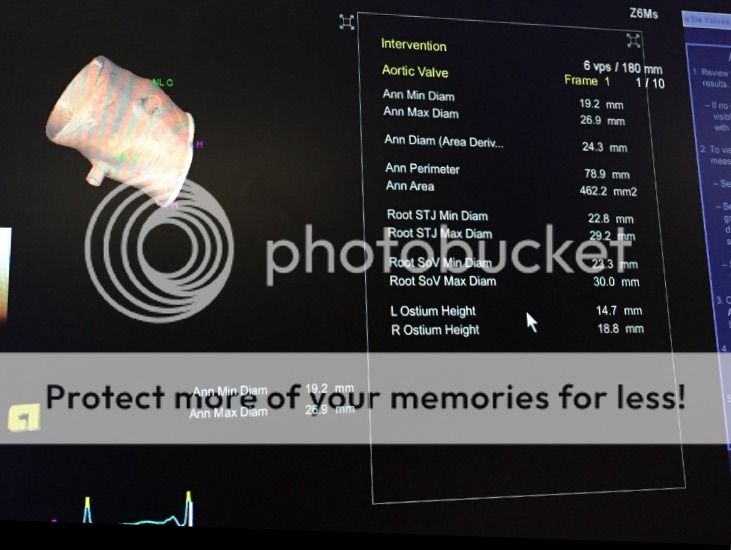
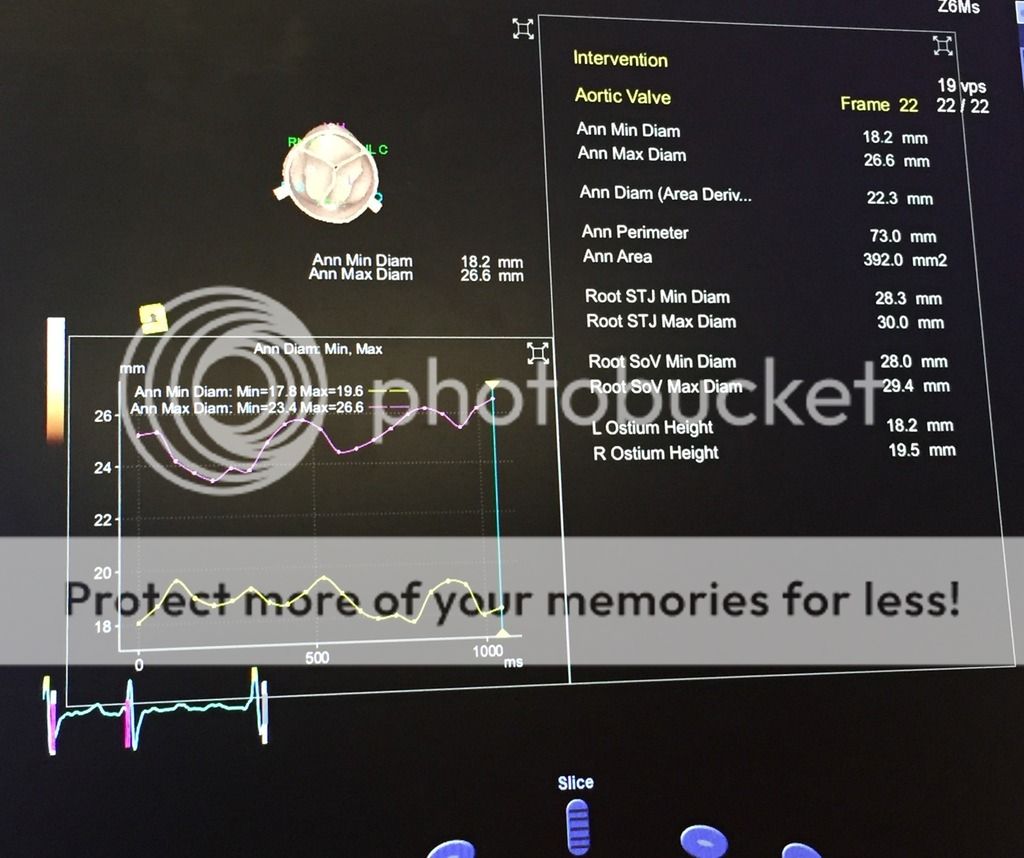
Anyone have good resources for teaching yourself 3D TEE?
seems like at recent meeting all are signalling the death knell of 2D, though i think that's extreme.
helps to have a good machine. we have two, and one freezes every time you try to do 3D
seems like at recent meeting all are signalling the death knell of 2D, though i think that's extreme.
helps to have a good machine. we have two, and one freezes every time you try to do 3D