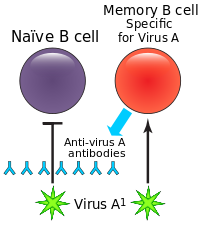
That is an interesting point, but I don't think that I would consider that potential problem to be unique to vaccination since that quirk of the immune system doesn't discriminate between exposure to a wild type pathogen and a vaccine. Vaccination does give us a little more control/influence in that we can continue updating vaccines and we can manage their administration. In contrast, we usually cannot pick which strains of an actively circulating pathogen a person will be initially exposed to and when that exposure will take place.It is theoretically possible that original antigenic sin could make a given vaccine bad, if it's some variant of a future, more virulent strain. Under this scenario, the new vaccine may be very ineffective, because of the previous vaccination. However, we cannot know this ex ante. Further, this can go both ways, in that early vaccinations can give somewhat of a lifelong immunity. I heard something happened like this for old people with respect to the recent H1N1 epidemic.
Last edited: