- Joined
- Jun 23, 2007
- Messages
- 3,816
- Reaction score
- 1,250
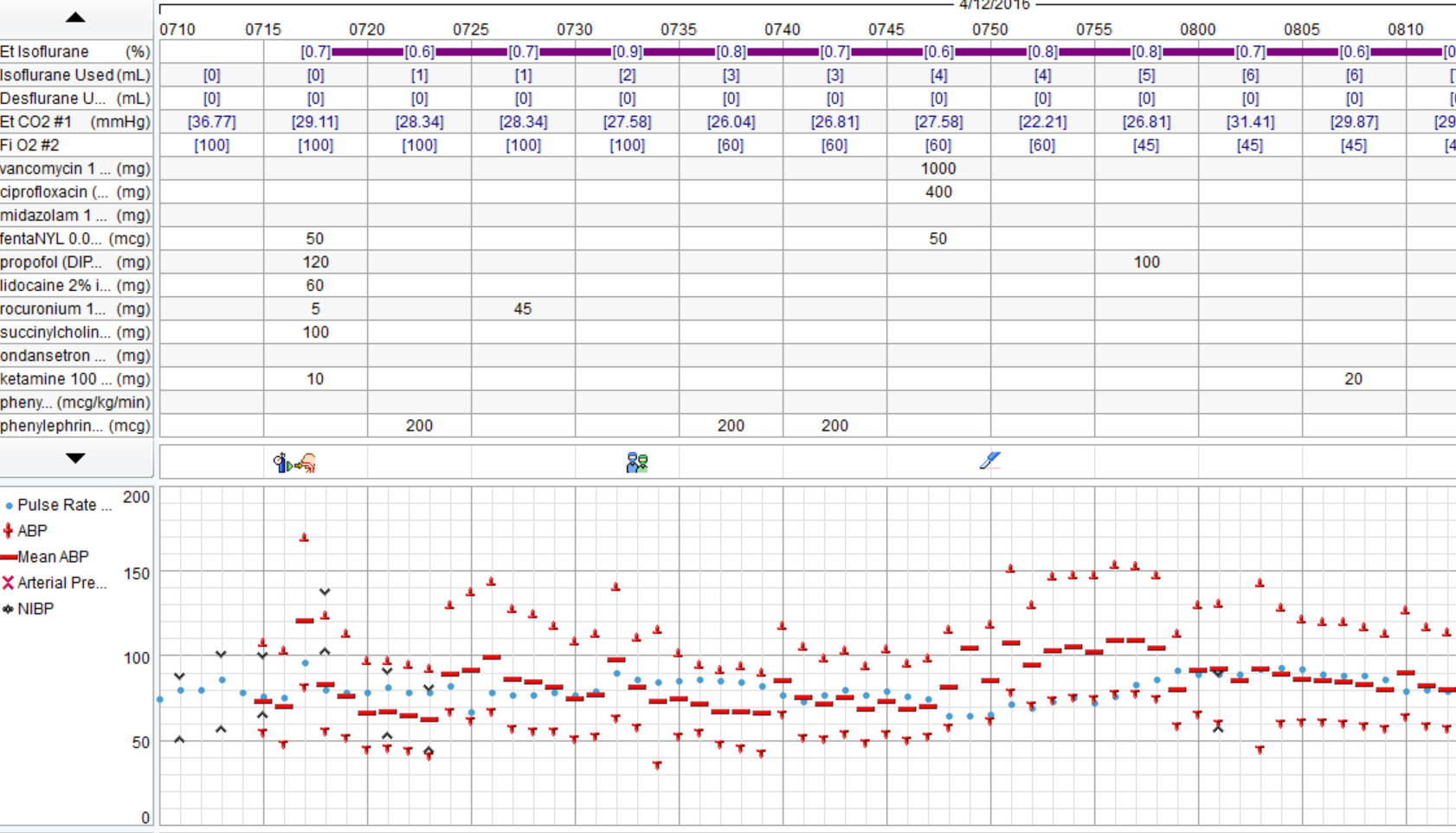
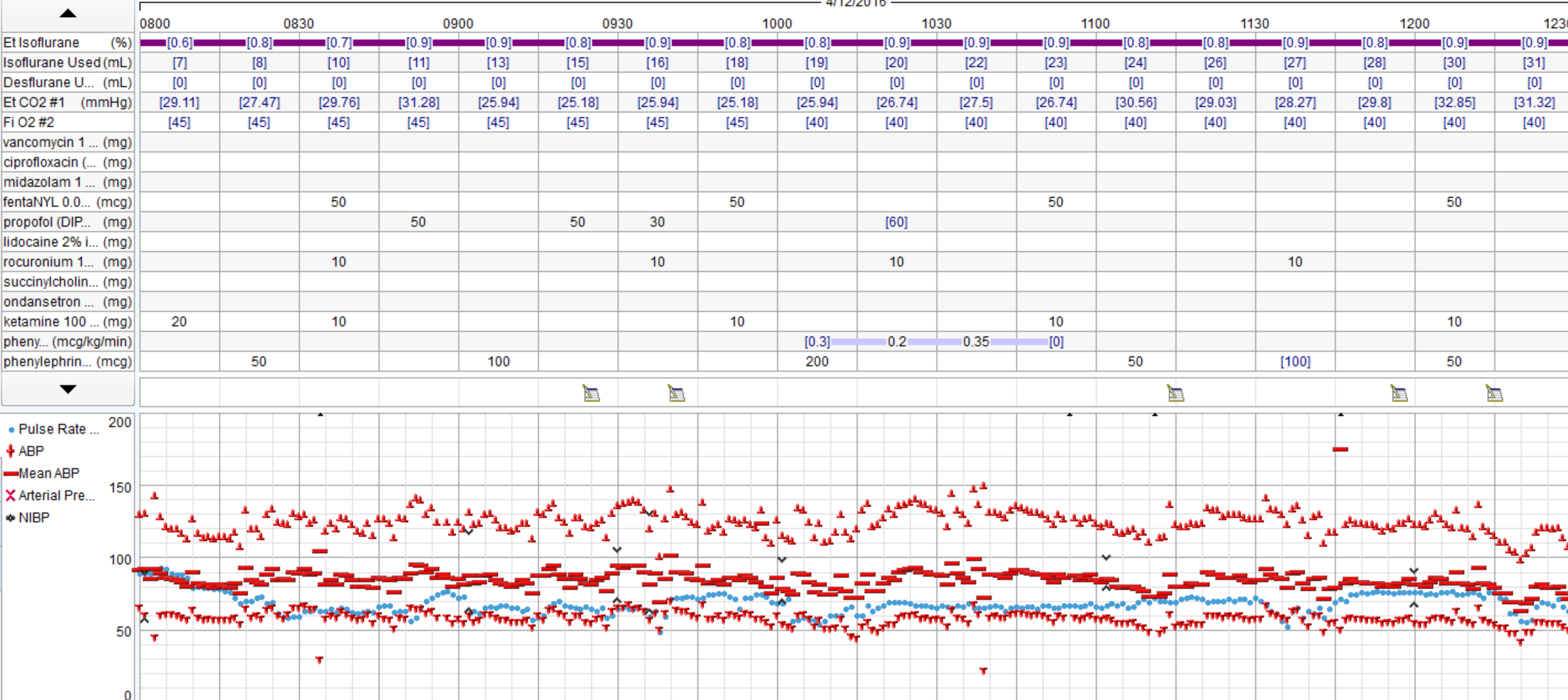
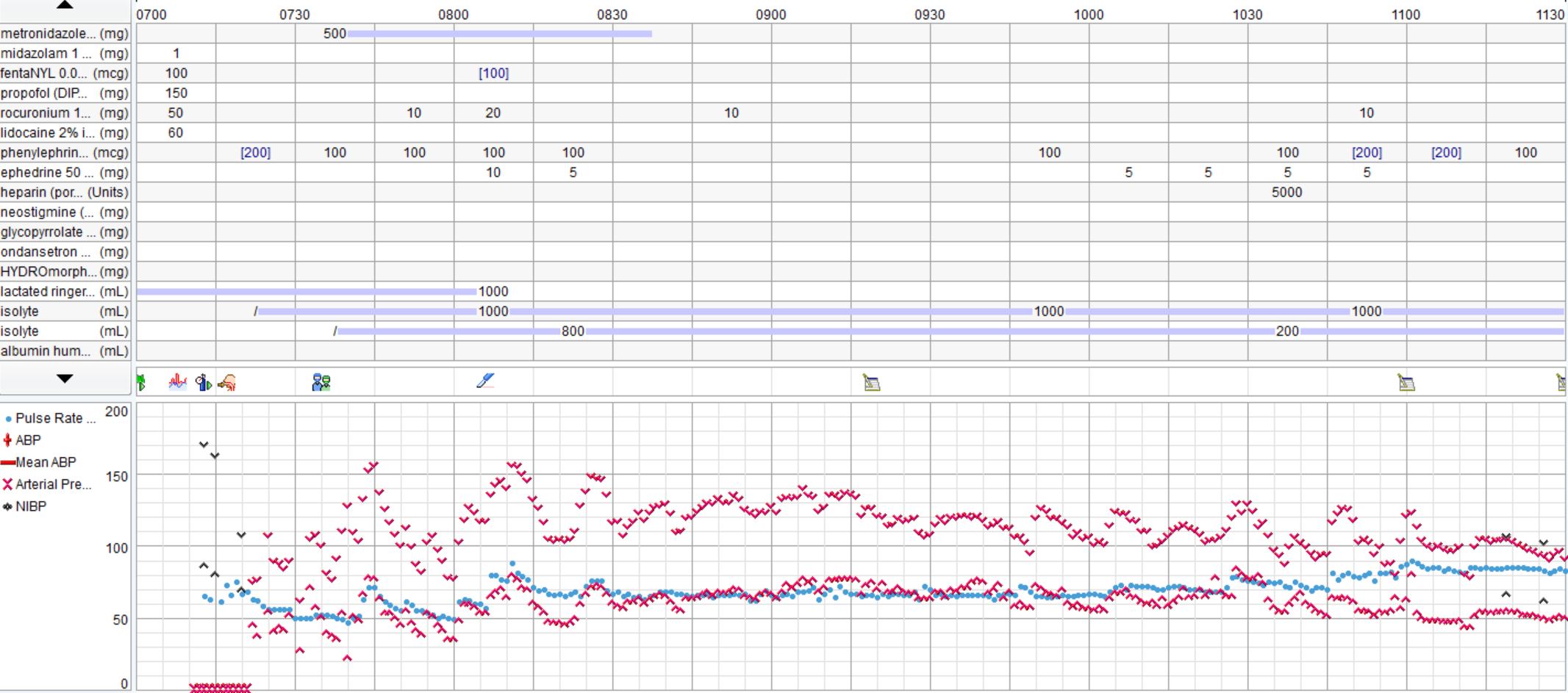
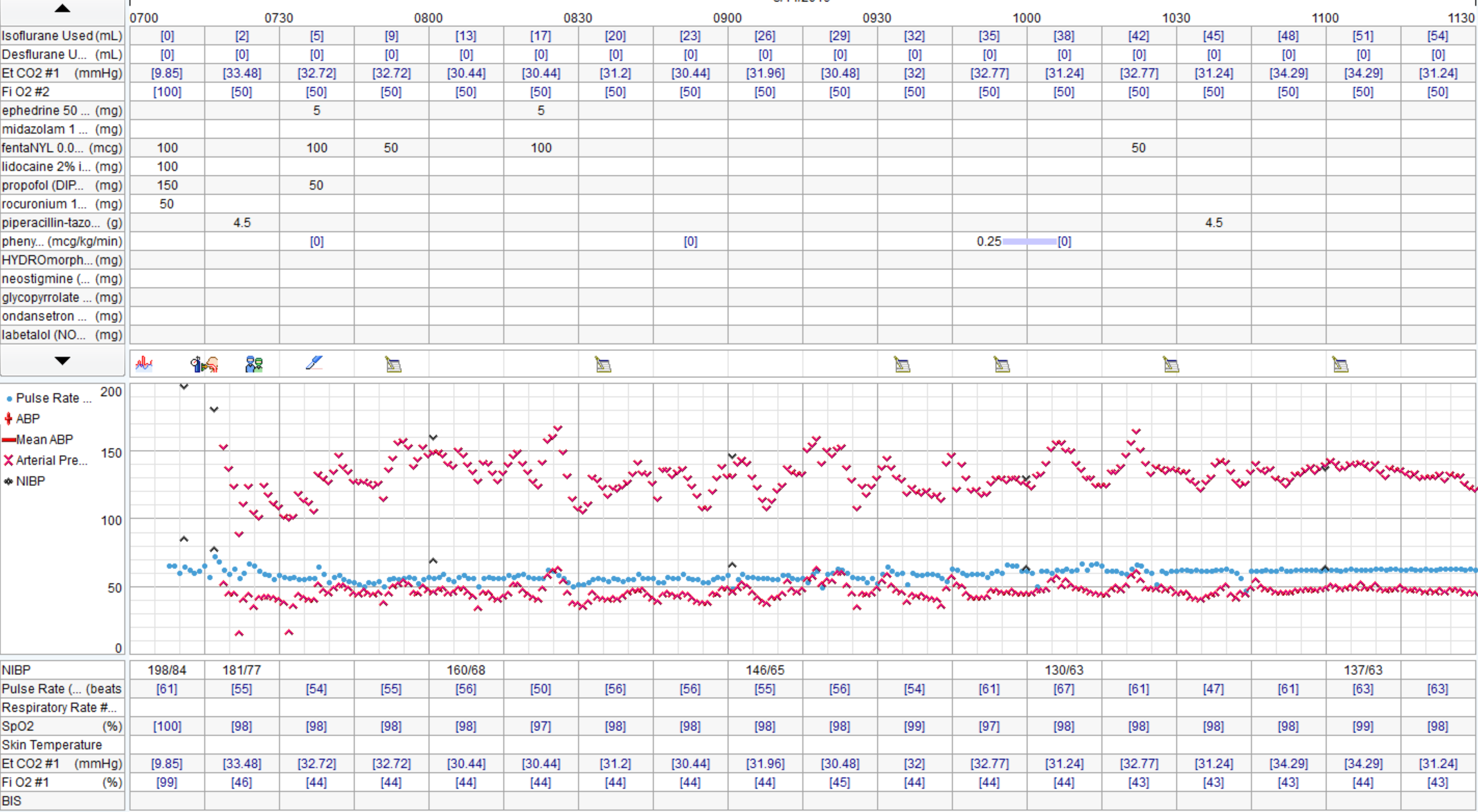
There was a severe deficit in the H&P.Good discussion. I agree that pt reports >4 METS and is undergoing low risk procedure, no EKG is warranted. None was obtained. In OR large P waves and occasional PVCs noted, otherwise no significant arrhythmias. Gentle induction with Propofol, easy LMA placement. Pt noted to be quite pale, pulse ox tracing lost. Anesthetist asks surgeon to do pulse check, surgeon states feels carotid pulse. Pulse ox noted to be off, replaced and return of signal with 100% O2 sat. Pt hypotensive (MAP approx 50). Pulse low 40's. 0.2 glyco and 5mg ephedrine given. MAP raised to high50's/low 60's, pulse increased to 60's. No further problems, BP continued to rise to baseline, 10 mins, case is over. Pt to PACU, alert and conversing without complaints. Anesthetist asks for EKG and talks to family. Wife states, "well, he's been very fatigued the last few weeks. He's passed out a few times and when we left the ER the other day he said his chest felt really heavy and was having pain in his ribs". Pt admitted, serial troponins rising, EKG showed RBBB, inferior infarction age undetermined and ST depressions V3-6. Pt transferred to medical center. 2 days later, 4V CABG.
The EKG discussion is academic.

 )
)