Epidural Blood Patch: A Rapid
Coagulation Response
Key Words: BLOOD, COAGULATION.
COMPLICATIONS, HEADACHE+pidUral patch.
To the Editor:
Postspinal headache can be treated with autologous blood
patch placed into the epidural space. The ability of this
epidural blood patch to relieve postlumbar puncture headache
accounts for the mechanism of action but not the
speed of the clinical response (1). In a controlled model
simulating the mixing of blood and cerebrospinal fluid
(CSF) at a dural leakage site, we have found that a clot
forms in an average of only 22 s. This is some four times
faster than even an activated clotting time.
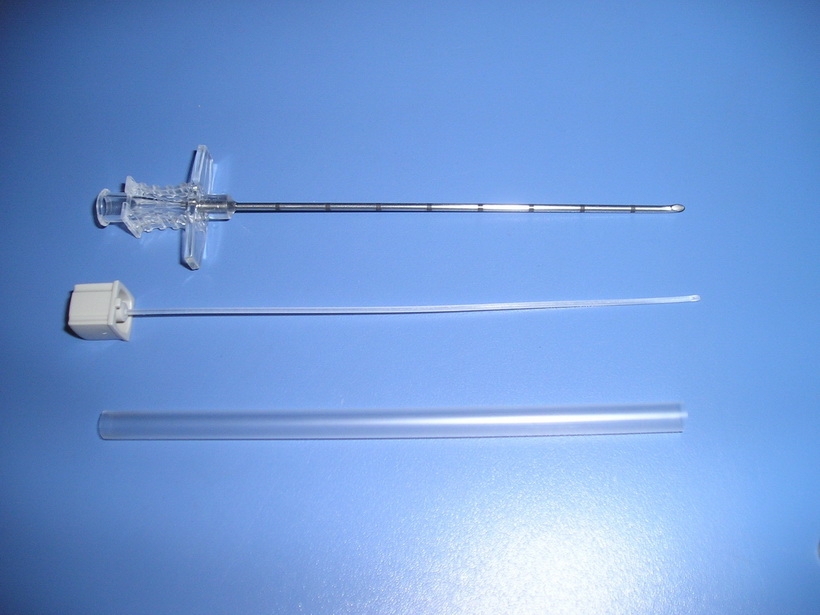
Method. A Litton Datamedix Thromboelastograph D
(TEG)2 was set up according to manufacturers instructions
and used to record the coagulation of unmixed blood and of
a CSF-blood mixture. Cerebrospinal fluid and blood samples
were obtained from six animals, with 360 pL of blood
being placed in a TEG coagulation pot and 180 pL of blood
followed by 180 pL of CSF mixed in a similar pot. These
were placed in the TEG and recording was simultaneously
begun at a paper speed of 2 mdmin.
Results. The results are summarized in Table 1. Variables
measured using a TEG include R, which represents onset
and formation of the clot via proliferation of coagulation
factors, the K-value, which represents the strengthening of
the clot by intrinsic plasma and platelet factors, and the R t
K value, which is equivalent to the clotting time. MA and
a-angle were measured, the former representing maximal
elasticity of the clot and the latter clot formation rate.
The R, K, and R + K values all showed significant
decreases, indicating an effect on coagulation and platelet
factors (2). Acceleration of the onset of coagulation and a
stronger clot were observed.
Discussion. It appears that when CSF and blood mix, an
acceleration of the coagulation cascade occurs. A previously
demonstrated procoagulant activity of CSF has generally
involved CSF altered by disease processes, pooled samples,
and coagulation activity of hemorrhage into CSF (3). We
used individual CSF samples and blood from healthy
animals without coagulation abnormalities. We used a TEG
that allowed us to show that it is mostly the R-time that is
affected in the formation of clot. In a previous study,
epidural blood patches were tested for leaks at a wide range
of CSF pressures, and, on examination of the puncture site
in the dural samples, some plugs were described (4). We
have observed a rapidity of clotting more in keeping with
the nearly immediate relief of spinal headache treated with
epidural blood patches, and suggest that there may be
coagulation at this interface of blood and CSF that causes
almost instantaneous formation of a plug. We believe the
reproducibility of our results, not seen in some previous
studies, can be attributed to careful control of the experimental
model. Human in vitro studies are planned.
Mark A. Cook, DO
J. M. Watkins-Pitchford, MD, FFARCS
Department of Anesthesiology
University of Michigan Hospitals
1 G32310048
1500 East Medical Center Drive
Ann Arbor, MI 48109