I recently received second hand advice from one of the pretty experienced attendings that to improve speed and efficiency, one should stop writing stuff down when talking to patients. I'm tempted to try it but worried I'm gonna walk out of the room and forget important **** for the HPI. Thoughts from anyone who has pondered something similar?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Fellow residents, do you take notes?
- Thread starter migm
- Start date
- Joined
- Feb 9, 2009
- Messages
- 560
- Reaction score
- 10
I would take notes all the time as a medical student. But now in residency I can't spend as much time in the room w each patient. If I only see 2-3 patients then go chart I can remember the story, but I don't go to long between charting on patients. Seems to just be a squired skill cause many senior residents and attendings can remember specific details on patients even hours or days later.
- Joined
- Oct 28, 2006
- Messages
- 3,105
- Reaction score
- 1,930
I stopped taking notes somewhere in the middle of medical school. Much like highlighting while reading, I found that it just turned into a distraction for me. When I abandoned note writing, I found that I walked away from the encounter with a much better overarching story of the patient rather than a bunch of discrete points I had jotted down. If it's a complex patient, I'll jot down a few details of the timeline or medications but this is rare.
I was prompted to try switching when a professor joked about medical students acting like they can't remember a 10 minute conversation without writing everything down but can memorize years of material for a standardized test...
I was prompted to try switching when a professor joked about medical students acting like they can't remember a 10 minute conversation without writing everything down but can memorize years of material for a standardized test...
I always take notes, but never on the hpi unless it's basic numbers like times they vomited or sometimes a pain scale.
My usual paper sheet is the following:
Pmd: -
Pmh: -
Psh: appy
Allerg: nkda
Sh: smoker, 25 beer a day, coke, ivda, heroin, Oxy, Xanax, soma, meth
My usual paper sheet is the following:
Pmd: -
Pmh: -
Psh: appy
Allerg: nkda
Sh: smoker, 25 beer a day, coke, ivda, heroin, Oxy, Xanax, soma, meth
- Joined
- Jul 9, 2008
- Messages
- 617
- Reaction score
- 49
Haven't taken any notes since I was a med student. But, to each their own so I'd just figure out what allows you the best combination of thoroughness + efficiency. Perhaps some sort of personalized 'Note-lite.'
- Joined
- Aug 18, 2007
- Messages
- 2,187
- Reaction score
- 511
The only notes I ever write down are phone numbers, doctor's name, maybe a med I never heard of.
If the patient told me they had 3 days of abd pain and I remember 2 days, I don't really care.
The chart is mainly there to cover my ass, not to transcribe what the patient told me.
If the patient told me they had 3 days of abd pain and I remember 2 days, I don't really care.
The chart is mainly there to cover my ass, not to transcribe what the patient told me.
- Joined
- Nov 2, 2004
- Messages
- 4,461
- Reaction score
- 5,244
In my 1st & 2nd year of residency I took notes, with the amount of information decreasing until it was minimal and only odd details, like what gman and render describe. So, while I think that the OP was given good advice, it should probably be phased in, rather than adopted precipitously and absolutely.
Nowadays I typically only use my pen to sign vicodin and valium prescriptions. The exception is when I'm working Fast Track and seeing & discharging 6 patients in a row before getting to do any charting. In those cases I'll write down a few things on the triage sheet and use it to jog my memory when I get a chance to come up for air and document the 3 ankle sprains, 2 back pains and a med refill I saw in the last 80 minutes.
I think something that's left out of the advice to the OP is the need to have a systematic approach in order to ditch the notes. I know that if I saw a back pain I considered cauda equina, epidural abscess and AAA, so I also know that I asked about incontinence, IV drug use and family history of AAA every time. Same goes for my physical exam. With that in mind, I might argue that it's not the absence of note taking that speeds you up, so much as it's having a differential diagnosis in mind before you even enter the room, and being able to rapidly work through it during your H&P.
Nowadays I typically only use my pen to sign vicodin and valium prescriptions. The exception is when I'm working Fast Track and seeing & discharging 6 patients in a row before getting to do any charting. In those cases I'll write down a few things on the triage sheet and use it to jog my memory when I get a chance to come up for air and document the 3 ankle sprains, 2 back pains and a med refill I saw in the last 80 minutes.
I think something that's left out of the advice to the OP is the need to have a systematic approach in order to ditch the notes. I know that if I saw a back pain I considered cauda equina, epidural abscess and AAA, so I also know that I asked about incontinence, IV drug use and family history of AAA every time. Same goes for my physical exam. With that in mind, I might argue that it's not the absence of note taking that speeds you up, so much as it's having a differential diagnosis in mind before you even enter the room, and being able to rapidly work through it during your H&P.
Last edited:
- Joined
- Aug 18, 2007
- Messages
- 2,187
- Reaction score
- 511
The advice above is spot on.
If you have a standard approach to each CC, remembering becomes much easier.
You only need to remember the pertinent positives and negatives.
Having a "red flag" approach to each CC, makes this process much easier.
If you have a standard approach to each CC, remembering becomes much easier.
You only need to remember the pertinent positives and negatives.
Having a "red flag" approach to each CC, makes this process much easier.
- Joined
- Jul 31, 2008
- Messages
- 294
- Reaction score
- 36
If you do need to take notes for your own sense of process, may I suggest you develop a system of bare bones short hand. This way you spend the least amount of time writing, can be perceived by the patient as being attentive, and your jinkies won't go crazy later thinking you forgot something. I haven't needed to take notes myself in a long time.
The closest thing I do now is I have an index card with patient name stickers on in that I carry in my pocket. I will write little things like CT or US to remind myself of what's pending without having to log into the computer system every 5 min's.
The closest thing I do now is I have an index card with patient name stickers on in that I carry in my pocket. I will write little things like CT or US to remind myself of what's pending without having to log into the computer system every 5 min's.
Ill play the devils advocate here. I think from a pts perspective if youre writing something down it appears you are paying attention. It gives another queue that you care. I dont write much now as a third year resident but a few key memory joggers seem to help. We dictate and often hours or gasps a day later. It certainly can help. Good luck
Sent from my LG-D801 using Tapatalk
Sent from my LG-D801 using Tapatalk
D
deleted547339
I take notes only when a patient has never been to the hospital before. If someone is new and has HTN, DM, HLD, COPD, CAD, CKD etc, I'll write down their meds. Usually those people have been to our hospital before, though.
- Joined
- May 3, 2004
- Messages
- 3,155
- Reaction score
- 3,750
No notes, and never use them. Pay attention to the pt and I actually think that scribbling down notes on a piece of paper while a pt is talking is distracting and makes it seem like you aren't paying attention instead of the opposite. Every been to a doc visit yourself where they have the terminals in each room and your doc is typing the note away while you talk, nodding all the while? Don't be that guy. Your memory for the details will improve with practice.
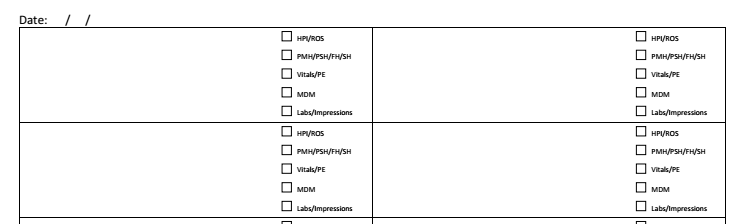
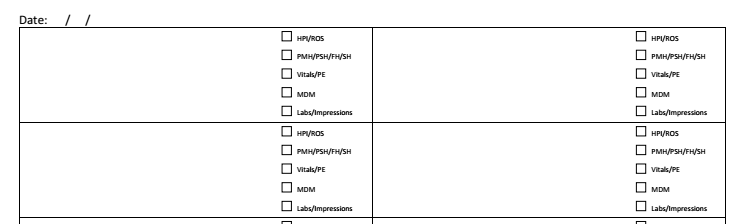
I have one sheet of paper that has boxes for patient stickers and check boxes to keep track of my notes (charting). I don't take notes in pt rooms unless its a single detail or two like a time / date or name that I'll forget
- Joined
- Dec 19, 2010
- Messages
- 10,254
- Reaction score
- 13,582
Here's my suggestion:
If you're going to take traditional notes on paper, go into the room with nothing larger than a sticky note pad. Divide your sticky note into fourths (draw large "+" on each sheet." Limit yourself to 1/4 of each sticky note per patient, ie, one square with "RM 7, chest pain, card work up, admit."
Next one, "RM 8, ankle, X-ray."
If you need more than that you're cluttering your head with useless nonsense, and you're going to look like a flea with a tome for each patient; that is all 3 that you saw per shift. You don't need to remember every fourth degree relative's CAD risk factors for your ankle sprain. Your shouldn't even be asking. So you forgot that on exam you noticed she had rheumatoid nodules on her hands. Who cares? You're an ER doctor and the patient is there for "ear hurts." Anything relevant, you will remember.
4 patients.
1 sticky note.
Need more?
Birdstrike fail.
.
.
.
.
.
.
(Exception: very sick patient. In that case you should throw your notes aside and maybe notice that your patient looks blue and might actually need a doctor; perhaps one confident in his airway skills and ability to perform critical life saving actions, such as yourself.)

If you're going to take traditional notes on paper, go into the room with nothing larger than a sticky note pad. Divide your sticky note into fourths (draw large "+" on each sheet." Limit yourself to 1/4 of each sticky note per patient, ie, one square with "RM 7, chest pain, card work up, admit."
Next one, "RM 8, ankle, X-ray."
If you need more than that you're cluttering your head with useless nonsense, and you're going to look like a flea with a tome for each patient; that is all 3 that you saw per shift. You don't need to remember every fourth degree relative's CAD risk factors for your ankle sprain. Your shouldn't even be asking. So you forgot that on exam you noticed she had rheumatoid nodules on her hands. Who cares? You're an ER doctor and the patient is there for "ear hurts." Anything relevant, you will remember.
4 patients.
1 sticky note.
Need more?
Birdstrike fail.
.
.
.
.
.
.
(Exception: very sick patient. In that case you should throw your notes aside and maybe notice that your patient looks blue and might actually need a doctor; perhaps one confident in his airway skills and ability to perform critical life saving actions, such as yourself.)
Last edited:
- Joined
- Dec 4, 2011
- Messages
- 1,847
- Reaction score
- 2,515
I agree with everyone else. You will look like a medical student if you take notes. I had one off-service resident who spent twenty minutes in a room and came out with both sides of a paper full of notes. I quickly realized he had no clue what was going on with the patient or what to do.
I do however walk around with a census with room numbers and jot down what side Xray I need to do because I can never remember that for the life of me. You could also jot down very specific (and limited) pieces of information that you may always forget to ask. This is more of a device to remember asking the questions and really only for billing purposes, i.e. Do you smoke, etc.
I do however walk around with a census with room numbers and jot down what side Xray I need to do because I can never remember that for the life of me. You could also jot down very specific (and limited) pieces of information that you may always forget to ask. This is more of a device to remember asking the questions and really only for billing purposes, i.e. Do you smoke, etc.
- Joined
- Jul 9, 2007
- Messages
- 1,199
- Reaction score
- 243
i agree with everyone, esp having a systematic approach.
at 1 hospital we have computers in the room and I chart while doing H&P so when they start telling stories about their last vacation and pets I am competing the entire chart, reviewing old charts, and checking on stuff, like if they already had labs/x ray done. if so they get dispo'd right there. I bring up x rays, show them lab numbers, tell them their rx.....etc. and hit print. I find they like it. you're spending a little time, answering q's. meeting the family...etc. just like a doctors' office. I seem them once, boss is happy, press ganey is happy, everyone's happy.
another bonus: my desk is literally in front of half the pod so it's beneficial to avoid the pts asking for coffee, bathroom, directions to mcdonalds and the oldie but goodie more pain medicine
the other place we don't have that and I am isolated from pt's so I print out the triage note before going in. it has meds, hx, vitals, chief complaint. do the h&p, follow a pattern, jot down stuff out of the ordinary, notes to myself like check previous stress test or give med, rx for hemorrhoids...etc, hit the important crap for billing like smoking/med/surg hx, and verify/refute what the nurse writes. do a few patients then go back to chart
at 1 hospital we have computers in the room and I chart while doing H&P so when they start telling stories about their last vacation and pets I am competing the entire chart, reviewing old charts, and checking on stuff, like if they already had labs/x ray done. if so they get dispo'd right there. I bring up x rays, show them lab numbers, tell them their rx.....etc. and hit print. I find they like it. you're spending a little time, answering q's. meeting the family...etc. just like a doctors' office. I seem them once, boss is happy, press ganey is happy, everyone's happy.
another bonus: my desk is literally in front of half the pod so it's beneficial to avoid the pts asking for coffee, bathroom, directions to mcdonalds and the oldie but goodie more pain medicine
the other place we don't have that and I am isolated from pt's so I print out the triage note before going in. it has meds, hx, vitals, chief complaint. do the h&p, follow a pattern, jot down stuff out of the ordinary, notes to myself like check previous stress test or give med, rx for hemorrhoids...etc, hit the important crap for billing like smoking/med/surg hx, and verify/refute what the nurse writes. do a few patients then go back to chart
- Joined
- Dec 4, 2011
- Messages
- 1,847
- Reaction score
- 2,515
One more thing: the job I'm starting at still uses T charts. I'll probably fill out the stuff I don't care much about in the room or stuff I forget to ask. This is just to complete the t chart and also so I don't have to make a second trip to ask "Oh I forgot to ask" questions. So I don't fill out HPI there since I remember that.
Also, remember that much of what the patient tells you is garbage anyways.
Also, remember that much of what the patient tells you is garbage anyways.
I ran out of room in my old note pad i'd been using when i started a couple months ago and switched to a much smaller note pad. now i have no room to write so i just remember most of it except for odd things as mentioned above or tricky timelines. Sometimes I'll check boxes on our Tsheets ROS, PMH, PSH, etc while talking just to save a couple seconds charting it later
- Joined
- Mar 6, 2005
- Messages
- 21,374
- Reaction score
- 17,895
My hospital recently opened up patient access to not just lab and imaging results but to notes as well. So I get messages from patients all the time telling me that they said they took 3 oxys every 4 hours, not the 4 oxys every 3 hours that I wrote in my note. I tell them I don't care but I assume this is going to bite me in the ass sooner or later.The only notes I ever write down are phone numbers, doctor's name, maybe a med I never heard of.
If the patient told me they had 3 days of abd pain and I remember 2 days, I don't really care.
The chart is mainly there to cover my ass, not to transcribe what the patient told me.
- Joined
- Aug 18, 2007
- Messages
- 2,187
- Reaction score
- 511
Scary.My hospital recently opened up patient access to not just lab and imaging results but to notes as well. So I get messages from patients all the time telling me that they said they took 3 oxys every 4 hours, not the 4 oxys every 3 hours that I wrote in my note. I tell them I don't care but I assume this is going to bite me in the ass sooner or later.
I'd never want patients seeing my notes.
Do the patients have a way to message you?
- Joined
- Oct 25, 2007
- Messages
- 136
- Reaction score
- 0
Why?Scary.
I'd never want patients seeing my notes.
Do the patients have a way to message you?
- Joined
- Sep 1, 2003
- Messages
- 529
- Reaction score
- 89
Why?
The truth hurts sometimes.
- Joined
- Mar 6, 2005
- Messages
- 21,374
- Reaction score
- 17,895
Yes, yes they do.Scary.
I'd never want patients seeing my notes.
Do the patients have a way to message you?
But I also discovered a way to not make my notes visible to the patient. I only invoke it on the crazy/demanding patients though.
And I should note that I'm not in EM.
- Joined
- Sep 17, 2014
- Messages
- 773
- Reaction score
- 1,456
Well this was a random bump. I had no idea people outside of medical students and IM residents took notes during patient encounters. I don't think I've wrote notes while talking to a patient since 2nd year of med school during standardized patient encounters. Taking notes is a waste of time, it's really not hard to remember the pertinent details in your 2-5 minute encounter with someone.
- Joined
- Dec 4, 2003
- Messages
- 1,239
- Reaction score
- 1,125
I have a small notepad that fits in my back pocket - Pretty much only the list in my own shorthand, unless there's a complicated timeline or other details. I mostly chart as I go, but am lousy at remembering which patient goes to which PCP, so that's the key piece of information (and usually the only thing) I write down, generally because I'm going to need it later to sort out who gets admitted to whom.
Room #) Last name, (PCP/other specialists)
Room #) Last name, (PCP/other specialists)
- Joined
- Aug 18, 2007
- Messages
- 2,187
- Reaction score
- 511
nice nerco-bump
There is no reason for a patient to see my notes.
Not because I write anything negative about a patient, I never do that.
It's just that I am not a court reporter.
I do not transcribe what they tell me.
There may be individual details which they perceive as not being accurate.
The reason I write notes are for medico-legal protection, billing and communication with other physicians. (in that order)
The history is usually a pretty brief synthesis of the case.
The bulk of the note is medical decision making, which a lay person would not be able to accurately interpret.
There is no reason for a patient to see my notes.
Not because I write anything negative about a patient, I never do that.
It's just that I am not a court reporter.
I do not transcribe what they tell me.
There may be individual details which they perceive as not being accurate.
The reason I write notes are for medico-legal protection, billing and communication with other physicians. (in that order)
The history is usually a pretty brief synthesis of the case.
The bulk of the note is medical decision making, which a lay person would not be able to accurately interpret.
- Joined
- Mar 22, 2009
- Messages
- 377
- Reaction score
- 190
Well this was a random bump. I had no idea people outside of medical students and IM residents took notes during patient encounters. I don't think I've wrote notes while talking to a patient since 2nd year of med school during standardized patient encounters. Taking notes is a waste of time, it's really not hard to remember the pertinent details in your 2-5 minute encounter with someone.
When I have 10 patients on my census with CP/SOB, helps to jot down some deets to help with charting and remembering who is who later. Really not that big of a deal.
- Joined
- Mar 13, 2012
- Messages
- 636
- Reaction score
- 659
I have a policy of finishing all paperwork and dictations before leaving a shift. It really sucks after a long shift were you go slammed, but the discipline is important. I used to "just do it tomorrow", but no longer.Ill play the devils advocate here. I think from a pts perspective if youre writing something down it appears you are paying attention. It gives another queue that you care. I dont write much now as a third year resident but a few key memory joggers seem to help. We dictate and often hours or gasps a day later. It certainly can help. Good luck
Sent from my LG-D801 using Tapatalk
First, you really do loose the finer details a day later. Second, it is all recorded in the EMR when you charted, so in a lawsuit, any decent lawyer will come after you and question your memory if they noticed you charted the encounter 3 days later, but if you dictated something smack in the middle of when the **** was hitting the fan, it can be a critical insight into your thought process and save you in court.
- Joined
- Mar 13, 2012
- Messages
- 636
- Reaction score
- 659
I agree with everyone else. You will look like a medical student if you take notes. I had one off-service resident who spent twenty minutes in a room and came out with both sides of a paper full of notes. I quickly realized he had no clue what was going on with the patient or what to do.
I do however walk around with a census with room numbers and jot down what side Xray I need to do because I can never remember that for the life of me. You could also jot down very specific (and limited) pieces of information that you may always forget to ask. This is more of a device to remember asking the questions and really only for billing purposes, i.e. Do you smoke, etc.
Agree, a sticker census is critical, mainly to remember where they are and a one word chief complaint. "CP, SOB"
- Joined
- Jan 2, 2013
- Messages
- 389
- Reaction score
- 319
I used to be a big note-taker, but I find that as I go through intern year I naturally remember most of the important stuff and write less and less. I still get into trouble sometimes when I'm juggling 3 or 4 pts with all the chronic diseases or old people with dizziness... which one was hospitalized 10 years ago for Actinomyces again? Which one is taking warfarin? Missing these things is poor form with most of my attendings, and our EHR is too slow to look them up again quickly, and anyway it's a rare day that a pt has an updated med list in the system by the time I see them. So, the fastest solution I have is to take notes.
So, don't stress about whether you take notes or not. You'll probably develop a better memory for these things as an intern.
So, don't stress about whether you take notes or not. You'll probably develop a better memory for these things as an intern.
- Joined
- Sep 1, 2003
- Messages
- 529
- Reaction score
- 89
When I have 10 patients on my census with CP/SOB, helps to jot down some deets to help with charting and remembering who is who later. Really not that big of a deal.
If you are trying to remember info on 10 patients, you're doing it wrong. Keep up with your charting then you just have to go back and reread your H&P if you can't remember which patient was which.
- Joined
- Mar 22, 2009
- Messages
- 377
- Reaction score
- 190
If you are trying to remember info on 10 patients, you're doing it wrong. Keep up with your charting then you just have to go back and reread your H&P if you can't remember which patient was which.
Keep up with your charting...why didn't I think of that!
Too many patients, not enough time. Charts must be done later.
D
deleted547339
Keep up with your charting...why didn't I think of that!
Too many patients, not enough time. Charts must be done later.
Learn to be more efficient. That's the answer. It's not easy, but it is simple.
D
deleted109597
Nope. If they're not actively dying, then you need to be charting contemporaneously. Otherwise, you're creating more work for yourself. I had to force myself to start doing this in residency (and fellow residents would get pulled out of conference for being weeks behind in charting). Chart as you go, not when you go home. Otherwise, you're working for free.Keep up with your charting...why didn't I think of that!
Too many patients, not enough time. Charts must be done later.
- Joined
- Sep 17, 2014
- Messages
- 773
- Reaction score
- 1,456
I like to chart as I go; however, it is impossible to do while attempting to get work ups started on the surge of patients that just came through the door while getting other patients dispo'd simultaneously. If you are wasting time trying to catch up on your charting, you're going to have a lot of delayed starts to work-ups and an eventual backup of patients. My goal is not just to manage my patients, but to help manage the department, as well. I find time to chart whenever I get time later in the shift. Luckily we have staggered scheduling so I can stop picking up patients in order to finish up my charting before I go. Also, I never leave without completing all my charts.Nope. If they're not actively dying, then you need to be charting contemporaneously. Otherwise, you're creating more work for yourself. I had to force myself to start doing this in residency (and fellow residents would get pulled out of conference for being weeks behind in charting). Chart as you go, not when you go home. Otherwise, you're working for free.
- Joined
- Mar 22, 2009
- Messages
- 377
- Reaction score
- 190
Learn to be more efficient. That's the answer. It's not easy, but it is simple.
I don't think it's a function of my efficiency so much as it is a function of me being expected to "run the rack" that is always, always, always full.
Nope. If they're not actively dying, then you need to be charting contemporaneously. Otherwise, you're creating more work for yourself. I had to force myself to start doing this in residency (and fellow residents would get pulled out of conference for being weeks behind in charting). Chart as you go, not when you go home. Otherwise, you're working for free.
You're right. It's just a matter of letting people wait and prioritizing charting. When I am more in control of how I work I will most likely adopt your way of thinking. For now....I'll just keep taking notes.
D
deleted547339
I don't think it's a function of my efficiency so much as it is a function of me being expected to "run the rack" that is always, always, always full.
You're right. It's just a matter of letting people wait and prioritizing charting. When I am more in control of how I work I will most likely adopt your way of thinking. For now....I'll just keep taking notes.
How many patients are you seeing an hour, on an average day?
- Joined
- Mar 22, 2009
- Messages
- 377
- Reaction score
- 190
How many patients are you seeing an hour, on an average day?
Yeah, I'm not playing that game.
- Joined
- Feb 23, 2010
- Messages
- 3,019
- Reaction score
- 6,120
???Yeah, I'm not playing that game.
- Joined
- Jul 4, 2006
- Messages
- 1,204
- Reaction score
- 1,078
I don't think it's a function of my efficiency so much as it is a function of me being expected to "run the rack" that is always, always, always full.
You're right. It's just a matter of letting people wait and prioritizing charting. When I am more in control of how I work I will most likely adopt your way of thinking. For now....I'll just keep taking notes.
Charting right away will likely help you be more efficient and might even allow you to see more patients over the course of the shift. The reason for this is that when you type up a chart immediately after seeing a patient it only takes a fraction of the time it would take later to either remember all the details if you aren't taking notes (was this the one that was on insulin or not?) or transcribe your notes to the EMR (what the hell did I write over here?).
- Joined
- Dec 4, 2011
- Messages
- 1,847
- Reaction score
- 2,515
Yeah, I'm not playing that game.
Cue early 90s rap song.
D
deleted547339
Yeah, I'm not playing that game.
I'm not playing any game. I was going to say that if you're seeing <2pph and not contemporaneously documenting, you need to be more efficient. If you're seeing significantly over 2pph, you need to slow down and document.
Trying to help, man.
D
deleted109597
I'm not arguing for you to sit there and write for 30 minutes while the charts pile up in the rack. I'm saying that once you get used to it, it makes you faster. I'm one of the top producers in the group (depends on how many nights I pull and which residents are there). I see patients primarily when the residents are having trouble keeping up. I'm not arguing for pie in the sky ideals, but real practices.I like to chart as I go; however, it is impossible to do while attempting to get work ups started on the surge of patients that just came through the door while getting other patients dispo'd simultaneously. If you are wasting time trying to catch up on your charting, you're going to have a lot of delayed starts to work-ups and an eventual backup of patients. My goal is not just to manage my patients, but to help manage the department, as well. I find time to chart whenever I get time later in the shift. Luckily we have staggered scheduling so I can stop picking up patients in order to finish up my charting before I go. Also, I never leave without completing all my charts.
If you're not charting after your shift then you're probably ok, but I promise you that you remember better while you're doing it as opposed to much, much later.
- Joined
- Mar 22, 2009
- Messages
- 377
- Reaction score
- 190
I'm not playing any game. I was going to say that if you're seeing <2pph and not contemporaneously documenting, you need to be more efficient. If you're seeing significantly over 2pph, you need to slow down and document.
Trying to help, man.
Thank you so much.
