With this mass effect on the trachea, I worry about tracheal collapse post-induction necessitating a sub-sternal trach.
I think it would be difficult to direct the tube to the left side in this case.
I've never put a DLT with FOB. I was thinking more along the lines of a tube exchange.
Also, if that deviation doesn't look bad, what does a bad deviation look like??
We have a CT of his chest, so it would be interesting to see what the actual path of his airway looks like, but that CXR just looks like a relatively small degree of deviation. The path just below the cords continues straight, and it appears to maintain width, while pushed slightly off to the right side, before coming back midline just above the carina. The fact that the trachea returns to midline may make proper placement of a left DLT more challenging, more so than the slight deviation itself. A few months ago, we had a guy here whose trachea made a greater than ninety degree turn off to the right just a few cm below the cords, almost crossed the clavicle, then turned again back toward midline. That was bad. Another thing to consider, would lateral mass effect from an aortic aneurysm necessarily lead to collapse of a cartilaginous structure with neuromuscular blockade? This is a real concern with sizeable anterior mediastinal masses, but there, the direction of force is different in a supine patient.
By the presentation, it does not seem as though we are crashing back to the OR to deal with an acute dissection, so I would first review the CT with the radiologist and/or surgeon, looking specifically at airway anatomy for evidence of compression, and other effects of an enlarged aorta on adjacent structures (esophagus). I would perform a directed history and physical, looking for any other cardiac history (given several risk factors), as well as any positional dyspnea, reflux, or other symptoms. He would get an arterial line, RIJ MAC, good PIVs, and a lumbar drain. I would also discuss with the surgeons if evoked potential monitoring would add anything to assessment of spinal perfusion, given the location of his thoracic aneurysm and previous AAA stent. I see nothing in his history so far that would be a strong indication for PAC. Provided no positional symptoms, no significant airway compromise on CT, and normal airway exam, he would receive a gentle vasculopath induction with neuromuscular blockade, with careful placement of a slightly smaller DLT (37 or 39), which would be guided into place via FOB down the bronchial lumen first. Assuming no GI pathology, I would also place a TEE probe.
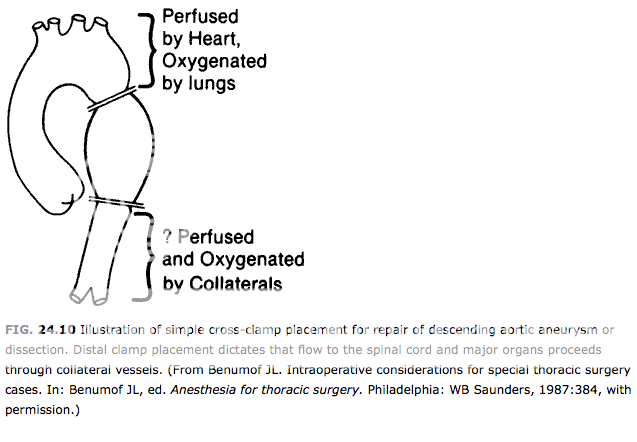
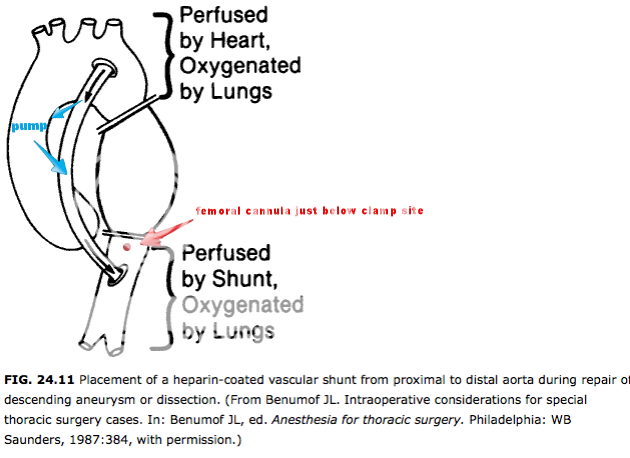
Is the surgeon willing to do this procedure quickly, with a high cross-clamp and no bypass, or are we thinking atrial-femoral bypass with either DHCA or ascending aortic cannulation as well, to keep the brain going? Also, where in his iliacs are his stents (and how recently were they placed), and what is the risk of femoral cannulation with iliac artery stents in place (may be a stupid question, but could the cannula snag part of a stent?)?