- Joined
- Apr 16, 2004
- Messages
- 4,660
- Reaction score
- 5,077
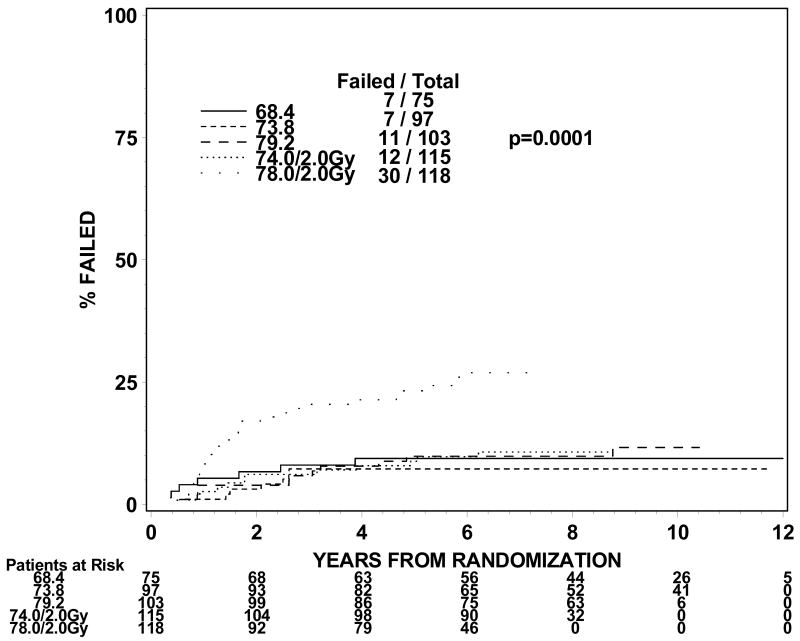
During residency, I've been taught that max small bowel point dose is 50.4 Gy. This was mainly based on Emami's original data. However, when I recently re-reviewed the QUANTEC paper on small bowel/stomach dose constraints, the max dose restriction appears to have mysteriously vanished. Specifically:
In recent RTOG trials, the max dose ceiling appears to have been lifted:
From RTOG 0848 (post-op pancreatic adenocarcinoma):
From 0524 (concurrent chemoXRT for muscle-invasive bladder cancer):
So under an 'ideal' scenario (no prior abdominal surgery, no adhesions) what is your comfort zone for max small bowel dose?
. . . if the entire volume of peritoneal space in which the small bowel can move is delineated, the volume receiving >45 Gy should be <195 cc when possible. Such a limit likely also reduces late toxicity risk, although this correlation is not established. The volume of small bowel receiving higher doses should also be minimized.
In recent RTOG trials, the max dose ceiling appears to have been lifted:
From RTOG 0848 (post-op pancreatic adenocarcinoma):
Max dose < 54Gy; D15% < 45Gy (no more than 15% of the organ can receive more than 45Gy)
From 0524 (concurrent chemoXRT for muscle-invasive bladder cancer):
Bowel: All attempts should be made to keep< 300cc's of the volume of the bowel receiving a dose greater than 45 Gy.
So under an 'ideal' scenario (no prior abdominal surgery, no adhesions) what is your comfort zone for max small bowel dose?