D
deleted171991
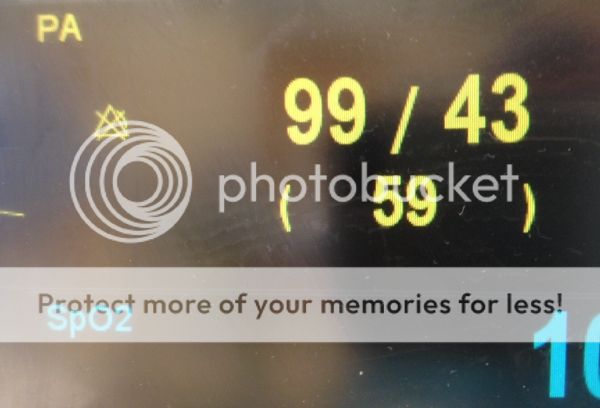
An article from the excellent Paul Marik, in the Annals of Intensive Care: "Obituary: pulmonary artery catheter 1970 to 2013" (via ScanCrit).
Food for thought. I personally hope that, in the future, all these invasive monitors will go the way of the bloodletting.
Conclusions
There is no evidence that the use of the PAC has improved patient outcomes. There are, however, convincing data that the hemodynamic parameters obtained from the PAC are inaccurate, are incorrectly interpreted and that these data frequently lead to excessive and inappropriate therapeutic interventions that maybe harmful. In addition, the data suggest that the hemodynamic parameters obtained from the PAC have little utility in managing critically ill patients in the ICU and operating room. These data therefore suggest that the PAC has a limited role in the ICU and operating room and challenge those experts who believe that the 'pulmonary artery catheter is still a valuable tool for hemodynamic monitoring'. The PAC, however, has a role in the diagnosis and operative management of patients with pulmonary hypertension and acute right ventricular failure.
Food for thought. I personally hope that, in the future, all these invasive monitors will go the way of the bloodletting.
Last edited by a moderator: