- Joined
- Apr 27, 2008
- Messages
- 4
- Reaction score
- 0
Hello,
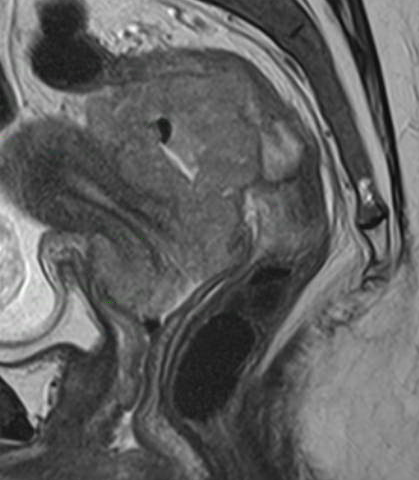
I am currently looking into the use of the Smit sleeve for the insertion of intrauterine applicators in HDR brachytherapy to see if they would be something that our centre would use. We have no practical experience regarding its use.
I have not found much literature discussing its use but I am still continuing with my research. Does anyone have any experience and opinion regarding its use?
So far, I have come up with a list of pros and cons:
Pros:
1. Eliminate multiple dilations of the cervix and hence less need for anaesthesia (1-2 vs 3-4)
2. Decreased risk of perforation (with closed end sleeve)
3. Shorter treatment time due to faster insertion
4. Less traumatic insertions (no seed markers needed, no need to grasp cervix)
5. Easier insertions for the brachytherapist
Cons:
1. Potential? patient discomfort/pain for 4 weeks (in addition to side effects from chemoRT)
2. Sleeve has to be sutured on cervix which can slough off and sleeve will not stay in place
3. Difficult/Not possible for advanced cases
4. Potentially more trauma/anxiety/anaesthesia esp. if sleeve does not stay in place
Thanks in advance. I look forward to the replies and discussions.
I am currently looking into the use of the Smit sleeve for the insertion of intrauterine applicators in HDR brachytherapy to see if they would be something that our centre would use. We have no practical experience regarding its use.
I have not found much literature discussing its use but I am still continuing with my research. Does anyone have any experience and opinion regarding its use?
So far, I have come up with a list of pros and cons:
Pros:
1. Eliminate multiple dilations of the cervix and hence less need for anaesthesia (1-2 vs 3-4)
2. Decreased risk of perforation (with closed end sleeve)
3. Shorter treatment time due to faster insertion
4. Less traumatic insertions (no seed markers needed, no need to grasp cervix)
5. Easier insertions for the brachytherapist
Cons:
1. Potential? patient discomfort/pain for 4 weeks (in addition to side effects from chemoRT)
2. Sleeve has to be sutured on cervix which can slough off and sleeve will not stay in place
3. Difficult/Not possible for advanced cases
4. Potentially more trauma/anxiety/anaesthesia esp. if sleeve does not stay in place
Thanks in advance. I look forward to the replies and discussions.