- Joined
- Mar 27, 2007
- Messages
- 114
- Reaction score
- 35
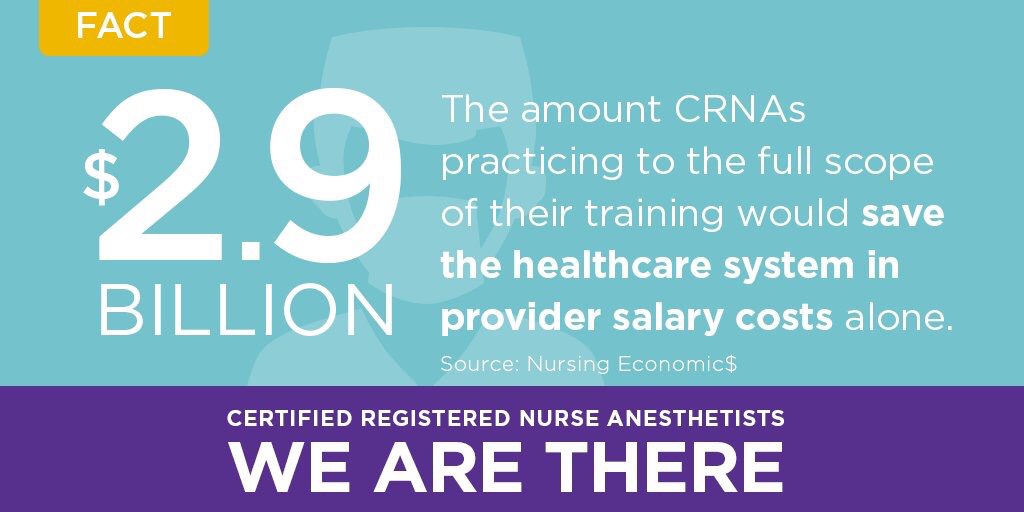
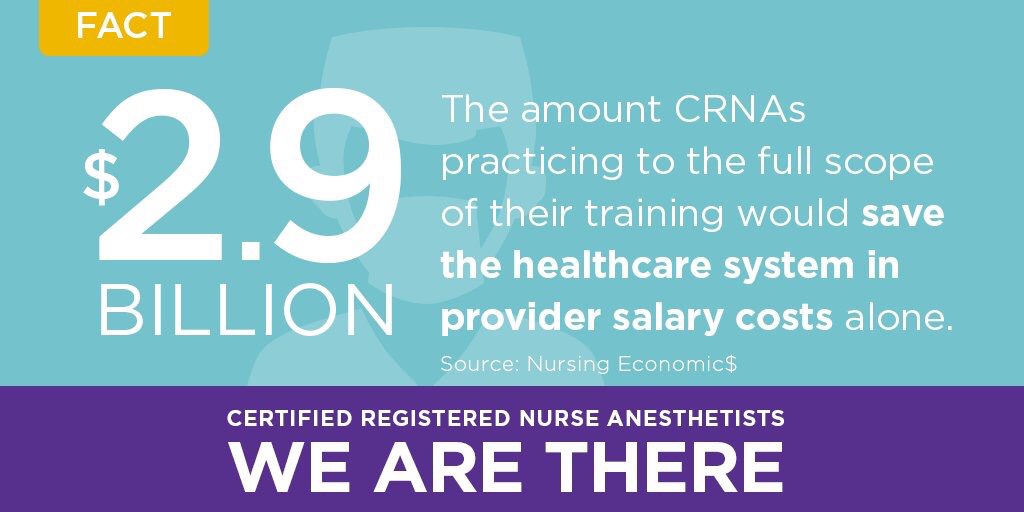
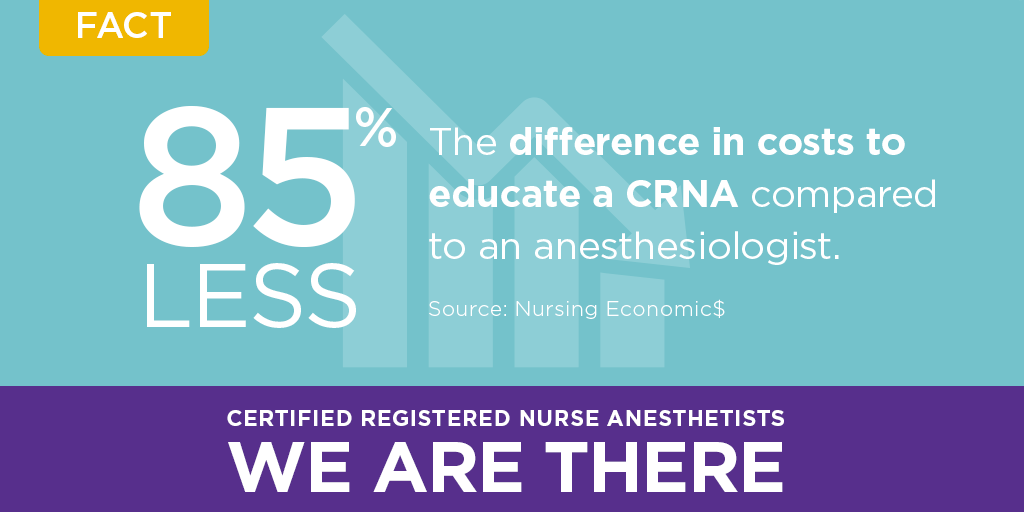
What anesthesiologists don’t want lawmakers to know:
#AnesthesiaFacts

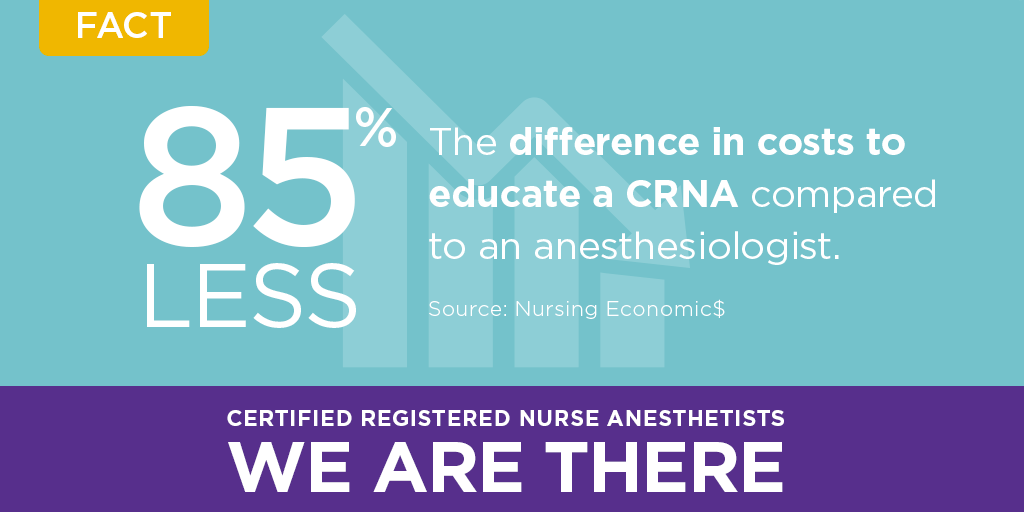
#AnesthesiaFacts


I’m calling BS.....they are implying that they are doing 9000 hours of anesthesia and they aren’t. They are trying to include all that RN time like it means anything to anesthesia...
This is their schedule, there is not 9000 hours clinical in it
Nurse Anesthesia - Plan of Study
I’m calling BS.....they are implying that they are doing 9000 hours of anesthesia and they aren’t. They are trying to include all that RN time like it means anything to anesthesia...
This is their schedule, there is not 9000 hours clinical in it
Nurse Anesthesia - Plan of Study
Lies on so many levels.According to their own statistics CRNAs receive around 2500 hours of anesthesia training and another 6500 hours of bedside ICU nursing experience to combine to make 9000 “clinical” hours.
Compare this to an average anesthesia resident who will perform between 12,000 to 15,000 hours of clinical training. If you add in the clinical requirements during medical school you probably approach 20,000 hours.
Its not just the hours of training but also the quality that counts. There is such poor quality of training for an SRNA that the thought they can be trusted to work solo is unfathomable.According to their own statistics CRNAs receive around 2500 hours of anesthesia training and another 6500 hours of bedside ICU nursing experience to combine to make 9000 “clinical” hours.
Compare this to an average anesthesia resident who will perform between 12,000 to 15,000 hours of clinical training. If you add in the clinical requirements during medical school you probably approach 20,000 hours.
Familiar with the CRNA vs. Physician issue but curious about actual recent legislation.
Has the AANA actually made any good ground on this subject? It seems like I see a lot of propaganda from them but little legislative action is translated. I feel like the AMA and ASA are both more powerful lobbies than any nursing lobby specific to anesthesia will ever be. Other than a few reprieves of allowing CRNAs to practice independently rurally, is there any other thing they have?
Yes, anesthesiologists train over 6 times in anesthesia but I don't think that is the primary difference dictating quality. IMHO the average anesthesiologists is superior because the selection process is more stringent. Usually top of the class in a real/competitive college degree. Top scores in standardized tests. Top of the class in med school. The average anesthesiologists who make it are so many standard deviations above the norm than any average nurse could ever come close even in their dreams.According to their own statistics CRNAs receive around 2500 hours of anesthesia training and another 6500 hours of bedside ICU nursing experience to combine to make 9000 “clinical” hours.
Compare this to an average anesthesia resident who will perform between 12,000 to 15,000 hours of clinical training. If you add in the clinical requirements during medical school you probably approach 20,000 hours.
Don't you think that is a huge part of it? Based on my experience (RN for 7+ years and soon to be an IM resident), I do agree that physicians have a much higher IQ than nurses on average.Yes, anesthesiologists train over 6 times in anesthesia but I don't think that is the primary difference dictating quality. IMHO the average anesthesiologists is superior because the selection process is more stringent. Usually top of the class in a real/competitive college degree. Top scores in standardized tests. Top of the class in med school. The average anesthesiologists who make it are so many standard deviations above the norm that any average nurse could ever come close in their dreams.
And that I think that matters when you are in deep doodoo.

Don't you think that is a huge part of it? Based on my experience (RN for 7+ years and soon to be an IM resident), I do agree that physicians have a much higher IQ than nurses on average.
In their minds they are “not your little brother”. They are your more pleasant twin.
P.S. The controller is not yours to give.
I don’t get the concept of tweets (Does that automatically exclude me from the millennial generation?). Who are they tweeting to? Who is reading these tweets? Do you really think that anyone other than the most aggressive CRNAs is following the AANA’s twitter account? What does the ASA tweet?
In other words, who cares.
I really hate saying “tweet” like it’s a serious thing worth paying attention to.
As I pointed out before: don't think about yourself as an intubator, central line placer, peripheral or spinal nerve blocker etc. Those are tech jobs and are slowly but steadily being taken away. Think about yourself as the doc who tells the techs what to do and carries the liability for it (and, again, your employer will want you to cover many-many techs). And if you don't want to teach your replacements, guess what? You'll be out of your job and somebody else will teach them anyway.Soon to be CA-1 here currently working in the ICU as a transitional year resident at community hospital.
So after reading this last night I come onto the unit today. Patient with a broken jaw and hemorrhaging from esophageal varices, needs urgent intubation. Anesthesia is called to bedside for intubation..... Guess who intubates this crashing patient while the anesthesiologist stands there teaching, the CRNA! We literally train them, not just how to push drugs in the OR, but even how to secure difficult airways, and then this is the **** that gets flung back at us. When will we stop training our replacements? How we can this kind of **** be said by their central organization one day and we still have anesthesiologists training them in advanced airways the next. This is crazy....
Excuse grammer/spelling, sent from iphone.
As I pointed out before: don't think about yourself as an intubator, central line placer, peripheral or spinal nerve blocker etc. Those are tech jobs and are slowly but steadily being taken away. Think about yourself as the doc who tells the techs what to do and carries the liability for it (and, again, your employer will want you to cover many-many techs). And if you don't want to teach your replacements, guess what? You'll be out of your job and somebody else will teach them anyway.
In my usual friendly manner, let me ask you: why were you so stupid to get into this specialty? What were you expecting? Why do you think CRNAs consider themselves a physician's equal? This forum is full of posts telling students to think twice before they jump. The body of American anesthesiology is full of cancer.
That is exactly why we are hired. Anesthesiology is increasingly becoming a field dominated by large employers (either AMC or the hospital itself) we are labor costs, the collected billing is the revenue. Your employer wants the cheapest workforce possible and that is 4:1 coverage (or more if they can get away with it). Your employer does not care about your personal opinion of CRNA’s or the future of anesthesiology. They want to cover the most rooms for the least cost. The only way to truly “fight” the CRNA takeover is to work for similar wages. I don’t see many docs volunteering for that so here we are....This attitude of seeing skills as monkey tasks is another reason why this this field isn't helping it's cause. Surgeons should be replaced by monkey techs too, how much brain power do you need to use a hammer and saw or carve things or cut flesh with a knife. I mean if you want to consider basic skills of your job as beneath you, why should a hospital hire us except for someone to take malpractice blame
That's pretty much how administrators think.This attitude of seeing skills as monkey tasks is another reason why this this field isn't helping it's cause. Surgeons should be replaced by monkey techs too, how much brain power do you need to use a hammer and saw or carve things or cut flesh with a knife. I mean if you want to consider basic skills of your job as beneath you, why should a hospital hire us except for someone to take malpractice blame
The skill of doing x y or z is easy enough! That's where nurses can compete with us.
It's when to do it and when not to it. They can't compete on that footing.
I know one paeds anesthesiologist who's never had a case of laryngospasm and I believe him... He's a wizard at avoiding **** ups before they happen. A 6th Sense, I don't know...
That's pretty much how administrators think.
Where is this idiocy with "top of the license", AKA top of the incompetence, coming from?
Soon to be CA-1 here currently working in the ICU as a transitional year resident at community hospital.
So after reading this last night I come onto the unit today. Patient with a broken jaw and hemorrhaging from esophageal varices, needs urgent intubation. Anesthesia is called to bedside for intubation..... Guess who intubates this crashing patient while the anesthesiologist stands there teaching, the CRNA! We literally train them, not just how to push drugs in the OR, but even how to secure difficult airways, and then this is the **** that gets flung back at us. When will we stop training our replacements? How we can this kind of **** be said by their central organization one day and we still have anesthesiologists training them in advanced airways the next. This is crazy....
Excuse grammer/spelling, sent from iphone.
I agree but the problem in surgery is that we are selecting intellectual people for a manual task. That's why imho i see so few talented surgeons.If I have surgery myself I wouldn't want anyone practicing "at the top of the license". First of all, what determines what they do with their license is through legislation not through skill or merit. Second of all, no physician ever says that about themselves - this is used by mid-levels "who call themselves advance practitioners" to make themselves sound good.
Bottom line is, I want someone who actually knows what they are doing. Practicing "at the top of the license" is not that.
That's pretty much how administrators think.
Why do you think it's not the surgeons who harvest the veins in a CABG? Why do plastic surgeons have PAs doing BIG parts of surgeries? Why did interventional radiology appear (and why are they also getting more and more PAs in the field)? Do you really think that, once technology permits, a lot of these manual tasks won't be delegated to people with better hands but weaker minds than ours? Where is this idiocy with "top of the license", AKA top of the incompetence, coming from?
Think like a capitalist owner would, not with your heart but with your wallet. It's happening in most specialties, but the easy procedural ones are most ripe for the coming revolution. It's mostly a matter of brainwashing the hoi polloi into accepting non-MD "providers".
Btw, I don't consider anything that I do solo as beneath me. Beneath my IQ and education? Yes (e.g. measuring urine, putting on monitors, moving and transporting patients, moving and setting up equipment etc., all the stuff that's a waste of a physician's time - and is done by nurses/techs in many other countries).
And don't fool yourself: surgeons will be replaced, too, as soon as it's possible. Just see interventional cardiology vs cardiac surgery. Btw, only fools would think that one needs a cardiologist with 7 years of GME to put in a stent or map an arrhythmia. Those are tech jobs, which don't need 99% of the medical knowledge of their practitioners. The two big things that protect physicians are the need for scapegoats and the lack of acceptance of "associate providers" by the masses. It's just a matter of time and easier to use technology (again, see the glidescope example). That's what we call PROGRESS, the biggest destroyer of jobs and occupations.
I understand what you are saying, but our society values people who DO things. There comes a point where you simply can NOT be seen by the public as just a supervisor. You must never lose your hands on skills or allow those in your perioperative environment see you as a non-DOER.
I get what you are saying but perception = reality. The perception by virtually ALL people is that DOERS are more valuable. Ignore this at your own risk.
One doesn't need to "do" everything. But, even the "monkey skill" of a cardiologist putting in a transvenous pacer will always be highly valued and the perception of value will be placed upon the person DOING the thing that saves the patients life, or is PERCEIVED by MOST humans to save the patients life.
We can intellectually masturbate all day long about "monkey skills" etc etc but this is nonsense in my opinion. Perception is reality. Period.
I understand what you are saying, but our society values people who DO things. There comes a point where you simply can NOT be seen by the public as just a supervisor. You must never lose your hands on skills or allow those in your perioperative environment see you as a non-DOER.
I get what you are saying but perception = reality. The perception by virtually ALL people is that DOERS are more valuable. Ignore this at your own risk.
One doesn't need to "do" everything. But, even the "monkey skill" of a cardiologist putting in a transvenous pacer will always be highly valued and the perception of value will be placed upon the person DOING the thing that saves the patients life, or is PERCEIVED by MOST humans to save the patients life.
We can intellectually masturbate all day long about "monkey skills" etc etc but this is nonsense in my opinion. Perception is reality. Period.
In addition to what individual anesthesiologists do, we as a profession need to fight back against the AANA's venom. Perception matters, I agree, and the AANA's incessant "we're as good as doctors" propaganda is meant to change public perception. The ASA won't do it. It thinks too highly of itself to sling mud like the AANA does.
I’m proud of my “monkey skills”. Its taken meAnd much as we would like medicine to be an intellectual endeavor, it is often “monkey skills”, applied quickly, that saves lives and prevents harm to our patients. Same goes for IR, surgery, interventional cardiology, etc. If you’ve ever worked with one who over intellectualizes and perseverates vs one that gets the job done quickly, you know what I’m talking about. The ones who have better monkey skills generally have a deeper understanding of the process and are able to filter out the noise from what is actually important. To quote @TempleChairman, anesthesia and much of procedural medicine is as much performance art as is is an intellectual endeavor. You need both. Sometimes on this forum we seem to undervalue monkey skills.
Ummm... You know CRNA salaries are less than half of Anesthesiologist salaries, right? Sorry to break it to you, but it hospitals save money by hiring them.
Sent from my BLN-L24 using SDN mobile
While the tweets are angering, maybe silently ignoring is the right approach after all? Let the little child yell, so far the powers that be have shown to understand the important difference... the employee always thinks he can do the job of the supervisor .. in any field... so what if they gain independence in rural BFE? No major city will ever yield..
If perception is all that matters, we have lost this battle a long time ago. Most of the public doesn't even know that anesthesiologists are physicians. 99% of my patients don't even blink when I tell them that I won't be in the room at all times (and these are ASA 3-4 patients). As long as the surgeon is OK with the person in the room, they are too. That's the sad reality.I understand what you are saying, but our society values people who DO things. There comes a point where you simply can NOT be seen by the public as just a supervisor. You must never lose your hands on skills or allow those in your perioperative environment see you as a non-DOER.
I get what you are saying but perception = reality. The perception by virtually ALL people is that DOERS are more valuable. Ignore this at your own risk.
One doesn't need to "do" everything. But, even the "monkey skill" of a cardiologist putting in a transvenous pacer will always be highly valued and the perception of value will be placed upon the person DOING the thing that saves the patients life, or is PERCEIVED by MOST humans to save the patients life.
We can intellectually masturbate all day long about "monkey skills" etc etc but this is nonsense in my opinion. Perception is reality. Period.
Independence for CRNA practice is not gained at the BFE level, but at the state level. While they publish their clearly skewed and biased 'studies' to use as as supporting proof for their claim about CRNA = MD, staying silent on the matter has been the practice that was used in the past. The result? 20+ states now allow independent practice for CRNAs. Its kind of like the colonial times where people who did not like the topic discussed simply abstained from voting, leading to the opposing party winning the topic, because the absentee votes did not infact voice their concerns.
The reason that AANA posts this BS is because no one challenges it because they think people/elected officials will have common sense. And therein lies the problem.
But the reality remains, although those 20+ states may allow it, it is not being done (at least that is my understanding) except in outliar circumstances. There are powers that keep the status quo. When my child yells, I ignore
Independence for CRNA practice is not gained at the BFE level, but at the state level. While they publish their clearly skewed and biased 'studies' to use as as supporting proof for their claim about CRNA = MD, staying silent on the matter has been the practice that was used in the past. The result? 20+ states now allow independent practice for CRNAs. Its kind of like the colonial times where people who did not like the topic discussed simply abstained from voting, leading to the opposing party winning the topic, because the absentee votes did not infact voice their concerns.
The reason that AANA posts this BS is because no one challenges it because they think people/elected officials will have common sense. And therein lies the problem.
There is a cult of ignorance in the United States, and there always has been. The strain of anti-intellectualism has been a constant thread winding its way through our political and cultural life, nurtured by the false notion that democracy means that "my ignorance is just as good as your knowledge."
- Isaac Asimov
He is right.
If perception is all that matters, we have lost this battle a long time ago. Most of the public doesn't even know that anesthesiologists are physicians. 99% of my patients don't even blink when I tell them that I won't be in the room at all times (and these are ASA 3-4 patients). As long as the surgeon is OK with the person in the room, they are too. That's the sad reality.
Also, you may think that most people value doers more (I don't), but that's not true for the bean counters. Bean counters know that doers are the easiest to replace, whenever technology allows (and that's where the midlevel revolution comes from). Anything that is simple enough to do will result in midlevel encroachment and worse. The future belongs to creative jobs, and that applies to medicine, too. Let's call them thinker-doers (e.g. the anesthesiologists who work in MICUs).
While we are used to wasting 20% of GDP on healthcare, those days are ending. In the era of cost-control, the concept of good enough becomes more and more important. Unless we add significant value to the healthcare product, we are not worth the added costs. Hence the continuously increasing coverage ratios. If seconds mattered so much to the bean counters, we would still have an anesthesiologist stool-sitting every patient in this country. Also, the number of anesthesia emergencies has decreased significantly with technological progress. Hence we depend on adding value by being able to do things a midlevel can't. And those are fewer and fewer, as years pass and technology advances. It doesn't matter if we do things better, if midlevels seem good enough, at least on paper.
Midlevels intubate, insert IVs, and even a-lines in most places. In some places, they are allowed to place neuraxial blocks. So what do we do? Central lines, peripheral nerve blocks, awake or difficult intubations, difficult (vascular, thoracic, cardiac) cases, and, most importantly, prescribe the anesthesia plans and take care of the patients postop. One solution is just to prevent them from doing all these procedures. That will last us a while, but not too long, not in the era when CRNAs matter more to department chairs than anesthesiologists (heck, I got reported by a PA for not teaching a central line to an APRN STUDENT during my fellowship). The other solution is to add more value, by developing more complex anesthetic plans. That may also work for a while. The truth is that it's very hard to beat somebody who has a decent IQ and has stolen your knowledge and experience for 10+ years, especially with all the technology. (That's not most CRNAs, but still a good number of them.) And THAT'S the coming reality.
Have you ever seen a CRNA do a case basically solo? Because if you have, you know that our role in the not so distant future is mainly to be the firefighters who fix all the stupid things they do do (and bean counters/surgeons don't get to see). Unless we agree to work solo for less, or figure out ways to add more value. Regardless, there will be fewer of us needed (while residencies are producing more and more of us).
I don't have a solution. I am probably safe, especially when considering my CCM backup. But the youngsters should realize that being a doer of relatively simple procedures coupled with mostly protocol-based medicine (which includes our famous "when seconds matter" situations) puts one at huge risk for being replaced by technology and less-educated workers (that applies to surgical ICUs too, by the way). One may keep being in denial, like all the workers whose occupations were replaced by technological progress in human history. Or DO something about it.
@GA8314, I think you give people too much credit. There is A LOT OF GREED in medicine. I would bet most of your colleagues would not give up that 100k as easily as you think given the option.
Problem with this BS “collaborative model” is 2 fold. 1) the docs are going to get dumped on with all the cases the CRNAs can’t handle. 2) what is the legal liability if a doc happens to be free and has to lend a second pair of hands in one of the CRNA rooms? I’m comfortable doing this for my partners because they’re not incompetent. Who knows what you’re going to walk into with a CRNA room where there has been zero physician input or involvement?No, the trend absolutely does not need to be one of a firefighter. This is precisely why I will NEVER allow my "monkey skills" to atrophy. Because when you maintain your monkey skills, you will always have a job. You may make less, but I (and I'm in a 90% supervision model) would argue that most of us in ACT models would take a 100k pay cut for the stress reduction and greater professional satisfaction of doing our own cases.
The end game for us may be "collaborative" and we can see how reimbursements go from there, but I submit that you can make a GOOD living sitting your own cases, and that the future need not be greater than 4:1. Indeed, I do not feel that I am alone in being willing to take a 30% pay cut if ratios were to grow beyond 4:1.
Also, do you realize how desperate administrations are to relinquish employment of their precious CRNA's?? They can't dump them onto us fast enough. Or onto an AMC..... We employ the CRNA's at my shop. We docs in my practice are not at risk of a job, but if we transitioned to a collaborative model (which we can all agree is the end game of the AANA, ,so in other words if the AANA gets their way entirely), then we would need LESS CRNA's not more.
For the juniors out there. I can say this because I eliminated my debt in less than 5 years post graduation. I strongly recommend you do this. It gives you a sense of freedom, and I am serious when I say I would take 100k LESS if the BS factor get's too big. I am quite certain I would enjoy my day much more this way, barring endoscopy....
Also, when you look at FTE data, you will see that for 40 hours per week, we are not THAT much over what a CRNA cost is. So, perhaps the beancounters will recognize a different dynamic in this area as well. But, no, the "future" is not one of "firefighters". Some groups may choose to go this way, but the market will then shift in other ways.
We are a neurotic bunch in medicine. But, the sky is not falling.
