Also very surprised, I would never get obgyn to touch a negative ultrasound or a hospitalist to admit intractable abdominal pain. Must work in fairytale land.
I would be careful about being this dogmatic. For context, I work primarily in the community with very hard nosed specialists who generally do not enjoy or appreciate talking/consulting with the ER.
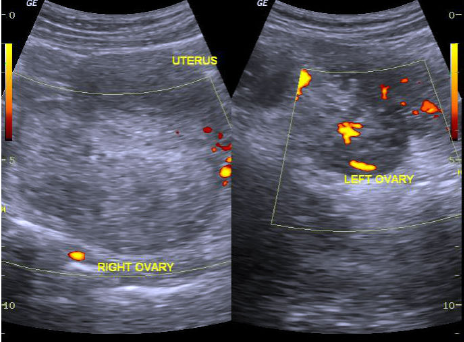
If you talk to any of the people on this board who have been doing this a long time I am sure they can regale you with many cases of imaging-negative, emergent pathology-positive situations. Torsions, ectopics, appys, choles, etc. Understanding the limitations of your tests is essential. None of our advanced imaging has 99% sensitivity.
It's all Baseyian statistics, the tests lower your post test probability, but if the pre test probability is very high (i.e. highly suspect history or physical exam), you may still not get to a sufficiently low level to "rule out" a serious problem. No we cannot rule out everything, yes there are atypical cases that will always be missed. But sometimes you get a classic story or gestalt seems right and the imaging is negative or equivocal, you have to pursue the next step.
In the community I would not call a specialist or surgeon until the imaging is done, but negative imaging is not 100% slam dunk, you're done. Diseases, particularly intraabdominal diseases are not simply positive or negative, they emerge on a continuum and early in their course they can be difficult to detect and the test characteristics are going to be poorer. It is not always completely unreasonable to admit patients for observation and tincture of time.
Not every patient with severe pain is "faking it." Malingering is a diagnosis of exclusion, and you cannot necessarily exclude every serious cause in the ER with the tests and time we have available. Severe intractable pain should be considered a red flag that raises clinical suspicion for serious pathology. If you have a patient with a low-normal number of ER visits in the last few years for normal things, my first thought is not "this person is a bull**** artist."
Obviously different patient with "10/10 pain" who looks completely comfortable on exam, with 12 ER visits in the last 6 months and 10 negative advanced imaging studies, allergies to all analgesics besides dilaudid, and who "somehow never can see the gynecologist," That's a different story.
Of course there are going to be questions of degree between those two hypothetical patients, but I think its probably prudent to assume the worse when it is unclear rather than immediately thinking the person is FOS.