In a true fellowship, the fellow functions mostly as a junior attending, directing residents and intervening only when they need help. That was my CCM fellowship (and many others'). Centering the fellowship on thinking and seeing as much as possible, not just manually doing, allows the fellow to be exposed to much more pathology and decisional experience. (We also had hundreds of hours for reading during my fellowship. Priceless.)
What I am beginning to see in ACTA fellowships is more along the lines of "superresidency", where the fellow is a glorified resident who just does cases. Fellowship is the time to focus on advanced TEE and case management, not to sit cases, IMO.
I have no doubt that what you're saying is true of CCM fellowships. Critical care is by its nature the care of many patients in parallel, and there's surely far more value for a fellow in the thinking and decision making ,rather than direct care of the patients in the rooms. The residents, interns, students, NPs, etc should be doing the information gathering, consult chasing, scut work, and most of the procedures.
I feel that cardiac is different and I deliberately chose a program where I would
not be supervising. (I'd also spent the previous years supervising residents as an attending, and wanted some alone time, so to speak.) A cardiac fellowship where the fellow actively supervises two residents at a time, increasing the number of cases the fellow is exposed to over the year, might have some advantages. But that doesn't actually appear to be the reality of the "supervisory" cardiac fellowships. The ones I talked to and visited had the fellows supervising one case at a time ... and you know what the fellows did when they weren't in the room? Had pretty relaxed days.
The advertised "value" of the supervisory programs was more time out of the OR during "boring" periods. But you know what? Much of anesthesia training is preparing for rare events, and avoiding them, and recognizing them quickly when they do occur, and handling them on your feet. And you've
got to be present to experience these events during training. I think we go a little overboard dismissing the stool-sitters, and I think every new grad would benefit from some time when they're doing their own cases solo and just have
time in the OR.
I'm a little weird in that I refuse almost every break I get offered. But I can't tell you how many times this year I've declined a break only to have a decision point, small or large, come up minutes later. Even during "boring" periods when nothing is supposed to happen. There's just no substitute for time in the OR, and everywhere I went that had fellows supervising residents, the fellows spent an awful lot of time not in an OR.
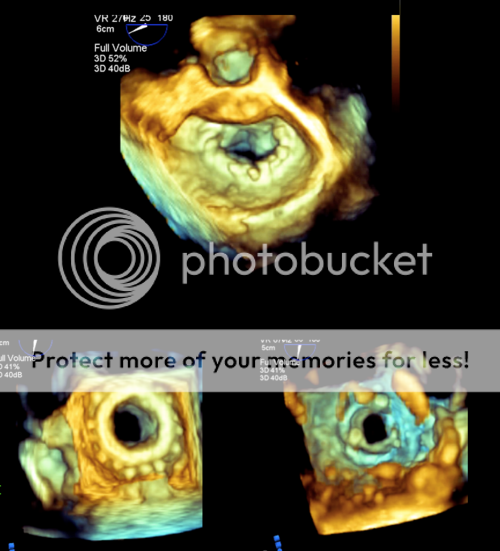
But they had plenty of time to look at pictures of echoes, and float through rooms to put their hands on probes.
I've supervised a resident about a dozen times this entire year, yet I've had superb TEE training and am approaching a certain comfort level with the sickest patients and most complex procedures (all the while being mindful of Dunning-Kruger pitfalls ... few people can be as dangerous as a doctor who's almost done with a period of training).
There have been times when I've felt overly micromanaged, and occasionally some days were filled with more work than learning, but if I had it to do over again, I still wouldn't choose an ACTA program that had more than occasional supervision.