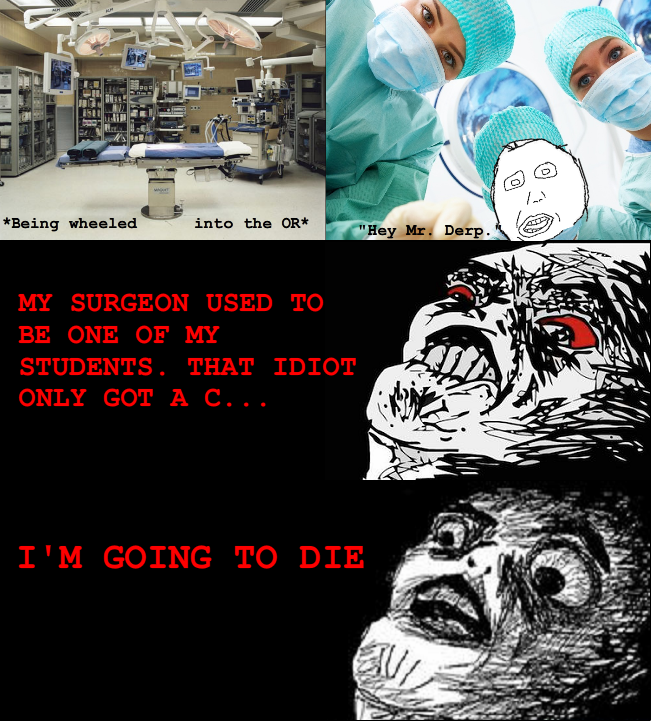
Nothing is worse than needing surgery, especially when you are a surgeon and know everything that can possibly ever go wrong. Last week I found my self in that situation. I had a huge pelvic mass (luckily turned out benign, path came back yesterday woohoo), and had to "go under the knife" with a gynecologist no less! I went it to it terrified of everything; not just the obvious, but worried about developing malignant hyperthermia, significant intraop bleeding, necrotizing soft tissue infections, DVT, PE, hernias, medication errors, etc. Everything i've ever seen or even read about I was sure was going to happen to me.
I chose my surgeons, I chose my anesthiologist, I even chose my scrub tech and circulating nurses. For the previous month I spent extra time at the gym, was at my idea body weight, I watched my diet and made sure I was eating high protein, high fat, etc. I did everything possible that was within my control to get the best outcome. The rest was out of my control. I do not enjoy not being in control.
Surgery came and went last week without any complicatons. I've been home since Friday. Here's what I learned from my experience.
1. I was terrified. I underestimate the terror that most of my patients feel when facing surgery. Most of them are undergoing more significant surgery and they are in worse medical condition than I am and are facing significantly bigger risk. They must be even more terrified.
2. Nurses are awesome. I've always respected nurses, but they truely are angels. When i had severe post op nausea and spent a night with my head in a basin, puking my guts up, the nurse was there, holding back my hair, washing my face and reassuring me that the nausea would get better. They called my surgeon in the middle of the night to get a Zofran order (i will never be annoyed at that call ever again). like she promised, the Zofran worked. When i came back from the OR with horrible puritis she got out a basin and washed off the prep that was irritating my skin. When she injected that incredibly painful SC heparin shots she explained how necessary they were yet apologized for the discomfort in a way that made me roll up my gown and take it. ... Nurses are wonderful people.
3. Don't underestimate the fatigue that goes with surgery. I thought i'd be back to normal in a week. I'm off pain killers, eating well, but I need a nap by 10am. I'm not a wimp. I have no idea why i'm so incredibly fatigued all the time. everyone keeps reassuring me this is normal after surgery. I have give the fatigue is normal speech many times, but i think i only half believed it. I don't know what it is about having someone cut a piece of you out that makes you need like 16 hours a sleep a day, but it does!!!
4. A laparotomy is a painful thing. It's not just the incision that hurts, it feels like someone ran over me with a truck. Because of the nausea I quit all analgesics except NSAIDs and acetominophen on POD2, but it still is way more painful than I ever expected.
So, I now have more sympathy for what my patients are going through. My pathology came back yesterday and is luckily benign. I will be back to work in another 2-3 weeks and will eventually get back completely to normal (except for the scar, and I haven't ruled out an incisional hernia yet). I don't think everyone has to have surgery to be empathetic and a good surgeon, but I'm trying to make this experience positive and help me understand what my patients are going through. Hopefully this will make me a better surgeon.
Just needed to vent; i'm going stircrazy here all day with nothing to do.
I chose my surgeons, I chose my anesthiologist, I even chose my scrub tech and circulating nurses. For the previous month I spent extra time at the gym, was at my idea body weight, I watched my diet and made sure I was eating high protein, high fat, etc. I did everything possible that was within my control to get the best outcome. The rest was out of my control. I do not enjoy not being in control.
Surgery came and went last week without any complicatons. I've been home since Friday. Here's what I learned from my experience.
1. I was terrified. I underestimate the terror that most of my patients feel when facing surgery. Most of them are undergoing more significant surgery and they are in worse medical condition than I am and are facing significantly bigger risk. They must be even more terrified.
2. Nurses are awesome. I've always respected nurses, but they truely are angels. When i had severe post op nausea and spent a night with my head in a basin, puking my guts up, the nurse was there, holding back my hair, washing my face and reassuring me that the nausea would get better. They called my surgeon in the middle of the night to get a Zofran order (i will never be annoyed at that call ever again). like she promised, the Zofran worked. When i came back from the OR with horrible puritis she got out a basin and washed off the prep that was irritating my skin. When she injected that incredibly painful SC heparin shots she explained how necessary they were yet apologized for the discomfort in a way that made me roll up my gown and take it. ... Nurses are wonderful people.
3. Don't underestimate the fatigue that goes with surgery. I thought i'd be back to normal in a week. I'm off pain killers, eating well, but I need a nap by 10am. I'm not a wimp. I have no idea why i'm so incredibly fatigued all the time. everyone keeps reassuring me this is normal after surgery. I have give the fatigue is normal speech many times, but i think i only half believed it. I don't know what it is about having someone cut a piece of you out that makes you need like 16 hours a sleep a day, but it does!!!
4. A laparotomy is a painful thing. It's not just the incision that hurts, it feels like someone ran over me with a truck. Because of the nausea I quit all analgesics except NSAIDs and acetominophen on POD2, but it still is way more painful than I ever expected.
So, I now have more sympathy for what my patients are going through. My pathology came back yesterday and is luckily benign. I will be back to work in another 2-3 weeks and will eventually get back completely to normal (except for the scar, and I haven't ruled out an incisional hernia yet). I don't think everyone has to have surgery to be empathetic and a good surgeon, but I'm trying to make this experience positive and help me understand what my patients are going through. Hopefully this will make me a better surgeon.
Just needed to vent; i'm going stircrazy here all day with nothing to do.