- Joined
- Jan 18, 2013
- Messages
- 152
- Reaction score
- 15
Hello dear friends,
I have a 60 yo patient, very fit that was diagnosed of a left NSCLC, that was resected and received adjuvant RT for N2 disease.
She did very well.
2 years later she developed 4 small nodules in the right Lung (controlateral) as only site for disease progression.
Biopsy revealed NCSLC , PDL-1+>90%.
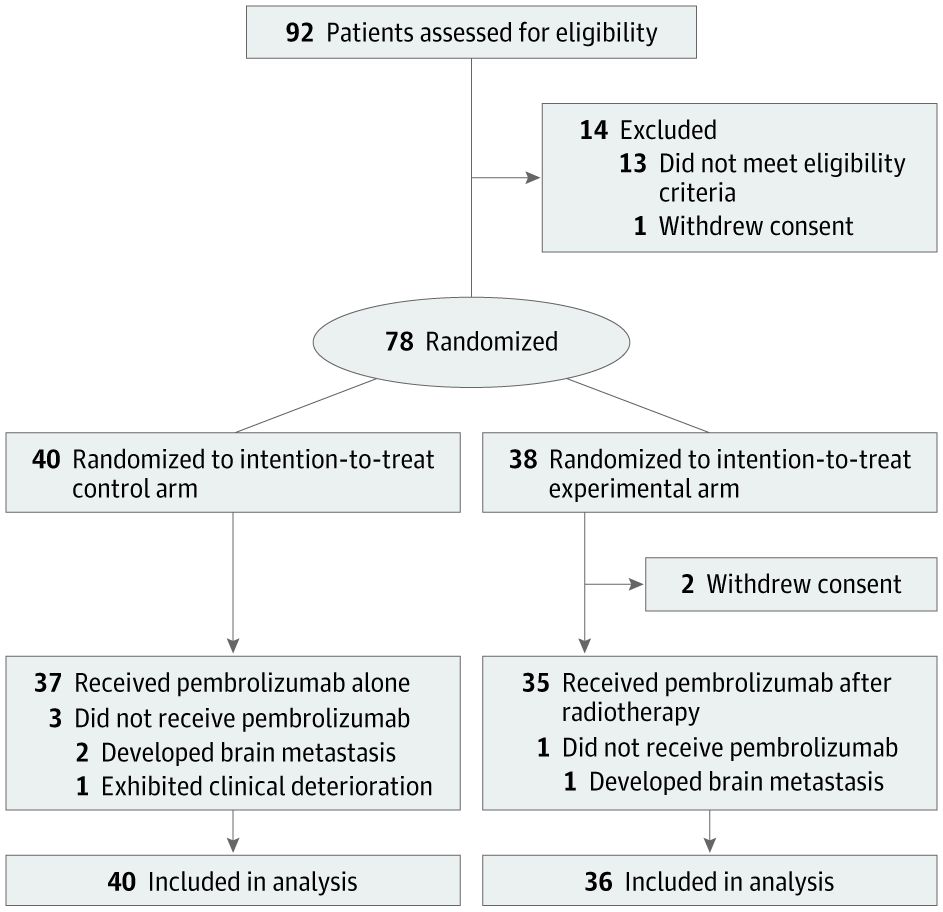
She received a Immunotherapy. at the follow-up, the number of lesions increased to 7 nodules. 2 out of 7 increased in size - with one adherent to the chestwall and that may become symptomatic soon.
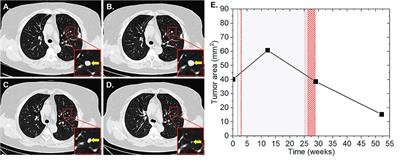
so we discussed to do a lung SBRT to the nodule near the chestwall to prevent from becoming symptomatic and to try to induce abscopal.
I know that per protocol, 50/5 is the best this subgroup.
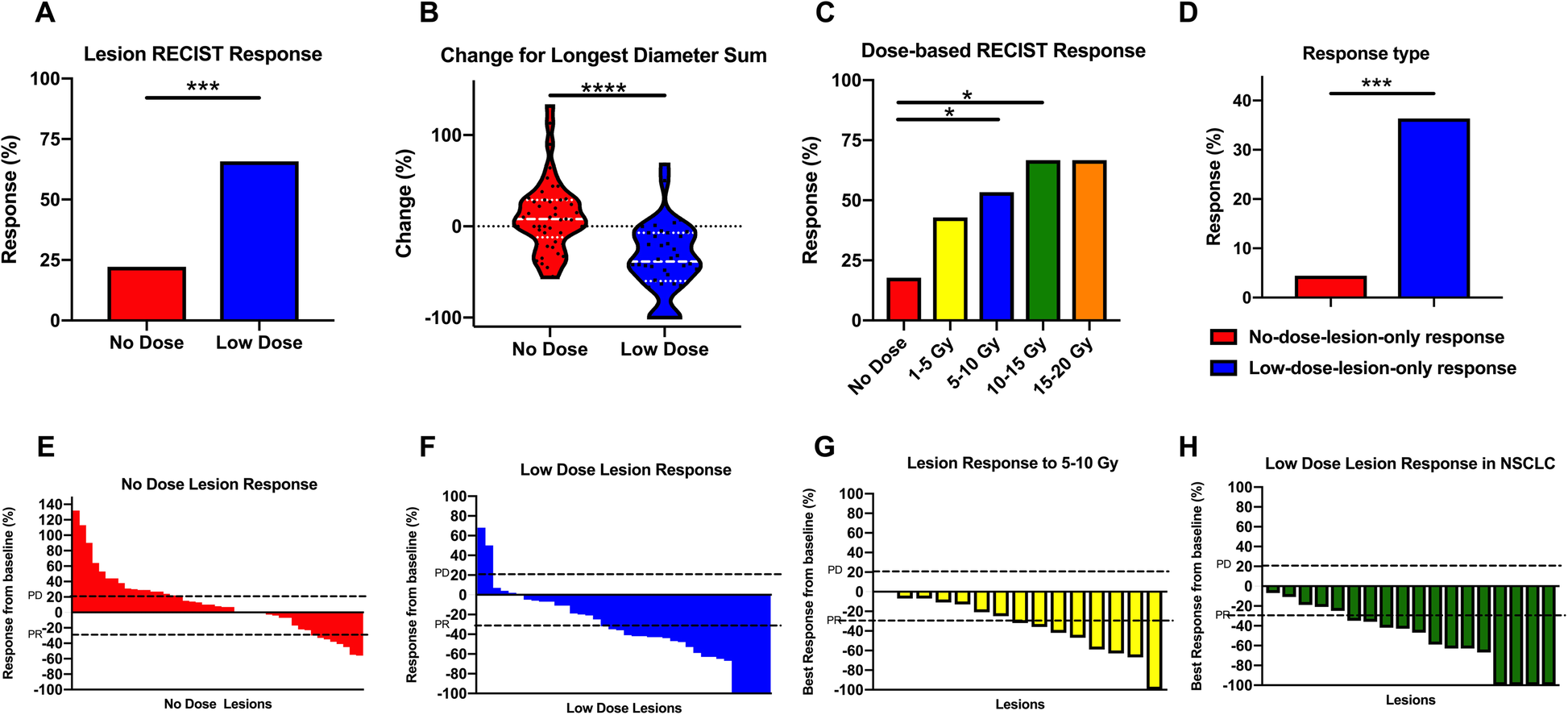
My concern is that maybe a lower dose per fraction would be more adequate for abscopal.
i would appreciate your feedback.
I have a 60 yo patient, very fit that was diagnosed of a left NSCLC, that was resected and received adjuvant RT for N2 disease.
She did very well.
2 years later she developed 4 small nodules in the right Lung (controlateral) as only site for disease progression.
Biopsy revealed NCSLC , PDL-1+>90%.
She received a Immunotherapy. at the follow-up, the number of lesions increased to 7 nodules. 2 out of 7 increased in size - with one adherent to the chestwall and that may become symptomatic soon.
so we discussed to do a lung SBRT to the nodule near the chestwall to prevent from becoming symptomatic and to try to induce abscopal.
I know that per protocol, 50/5 is the best this subgroup.
My concern is that maybe a lower dose per fraction would be more adequate for abscopal.
i would appreciate your feedback.