D
deleted87716
I’m curious what EM thinks should be the solution to shortages in the ED’s.
PAs.
I’m curious what EM thinks should be the solution to shortages in the ED’s.
So what are the take home messages here? Should FM not practice in the ED? Or what are we trying to get at here? We are all attacking Leroy’s comments but I’m curious what EM thinks should be the solution to shortages in the ED’s.
The solution to the shortage of EM physicians is more EM residency spots because only an EM physician should practice in an ED. Nevermind, that will decrease salaries of EM physicians.
The solution is FM doctors who are already in place and doing just fine. Nevermind, that’s not fair to people who did a residency in EM, and they will take EM physicians jobs.
Okay the solution is PAs. Wait, they shouldn’t practice independently in rural areas where EM physicians won’t go.
Ok the solution is independent PAs and NPs. Nevermind, they will take EM physician jobs from EM physicians because that’s entirely possible.
Honestly, it doesn’t matter what EM physicians think because they are employees without any control of their speciality.
How would that work, exactly? Incomes in medicine aren't based on supply and demand. They're based on reimbursement.
.
I’d say more specifically that cmg/hospital profits are based on reimbursement and what they have to pay a doc to bring that money in is actually based on supply and demand
It wouldn’t matter if a doc created $10mil in billings if the hospital had a line out the door willing to work for $85k
I’d say more specifically that cmg/hospital profits are based on reimbursement and what they have to pay a doc to bring that money in is actually based on supply and demand
It wouldn’t matter if a doc created $10mil in billings if the hospital had a line out the door willing to work for $85k
Yes.
How would that work, exactly? Incomes in medicine aren't based on supply and demand. They're based on reimbursement.
How are "FM doctors who are already in place and doing just fine" going to take jobs away from EM physicians? Presumably, those jobs would've already been taken by EM physicians if anyone wanted them. And, since when did "fairness" have anything to do with any of this? Life isn't fair.
No, but they can practice under supervision, which is pretty much how it's always done.
I don't know of any physician with two neurons firing simultaneously in their brain who thinks independent midlevels are a good idea, much less a solution to the physician shortage.
So are most FPs these days, in case you haven't noticed.
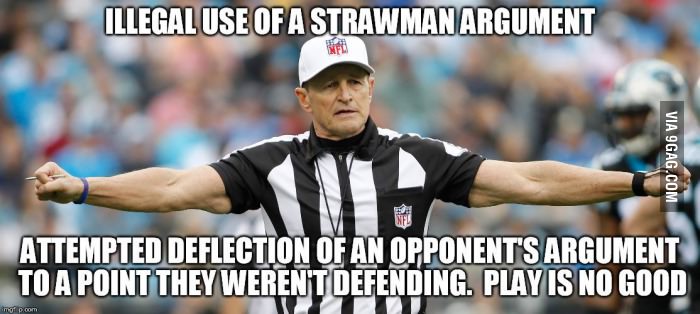
It's a straw man argument.
I think the problem here is you really enjoy quoting and bolding text.
Leroy -
What is the point of ABPS?
Do you think FM docs who complete a one-year EM "fellowship" (in an clearly inferior training environment) should apply for ABPS "board certification"? Should this FP doc then advertise as "board certified in EM"?
If you are truly just concerned with becoming a better FP physician to better care for patients in rural and otherwise underserved emergency departments, I am sure you would agree that all that is needed is the "extra year" (it's not really a fellowship in the traditional sense) of training. ABPS is just superfluous, right? Just a distraction, a money grab?
You certainly wouldn't use it or encourage others to use it to misrepresent and perhaps "trick" employers, would you?
HH
Could someone come along and create a new specialty, with even more ED training than current EM residencies and enforce a new standard?
Hypothetically, sure. Family doctors could add three years of surgical training, trauma, EM, OBGYN, etc to their training and be the new standard. (blah, blah, blah...)
[sarcasm] Um...yeeeah. That's not a straw man argument at all.[/sarcasm]
I don’t think you know what a straw man argument is.
Am I supposed to defend the ABPS? I could care less about that organization.
In an attempt to answer your question, the purpose of certification by a board is to uphold a certain standard. In this case, the standard being three years of FM residency and one year of additional training in EM under boarded EM physicians at a trauma center followed by an exam. Whether or not that standard means anything is up to the hiring organization to decide. From what I can gather, the vast majority of EDs in the US are okay with that standard.
Is EM residency an even higher standard? Probably so, certainly more recognized currently. Also has a board certification process with an exam etc.
Could someone come along and create a new specialty, with even more ED training than current EM residencies and enforce a new standard?
Hypothetically, sure. Family doctors could add three years of surgical training, trauma, EM, OBGYN, etc to their training and be the new standard. They could call their new specialty something sexy like disaster medicine. Then all of the sudden EM is left in the cold. Can you believe the EM guys only train for three years? What a joke. The disaster medicine guys can handle anything and train for six years. Every hospital needs someone boarded in disaster medicine.
Then EM docs would be the new second class citizens, and their board certification wouldn’t mean as much. This is all very fluid and employers opinions change.
The ABPS is simply upholding a standard. If you think it’s a joke, go sit on a hospital board, tell everyone it’s a joke, and don’t hire those docs.
Funny, because there was literally a thread a month ago about an FP who took a job at a level II trauma centre and got frazzled because they were utterly unprepared for the job despite the hospital credentaling them anyway.
Other - ABFM, Now Want ABEM
Lets trust non-clinical hospital admins to decide who is appropriate to work in what clinical setting - because clipboard pushers have so much insight into clinical practise, right?
Incorrect logic. Can’t discount the quality of EM residency because an ABEM doc somewhere has done terrible and got sued.
Incorrect logic. Can’t discount the quality of EM residency because an ABEM doc somewhere has done terrible and got sued.
This is a FM trained medical director who misjudged the acuity of their own ED and hired an FM trained attending who misjudged their own capabilities to work in an ED, and is now trying to address the deficits in their knowledge and skills by shadowing EPs at a Level I while effectively working as a midlevel.
Bonus points for the guy who got 30 OR tubes in a year-long fellowship and now feels "confident" to manage airways in the ER where patients are not NPO, often in C Collars with unknown PMHx and actively vomiting into their nonrebreather while satting in the 70s.
Goat. Rodeo.

The solution to the shortage of EM physicians is more EM residency spots because only an EM physician should practice in an ED. Nevermind, that will decrease salaries of EM physicians.
The solution is FM doctors who are already in place and doing just fine. Nevermind, that’s not fair to people who did a residency in EM, and they will take EM physicians jobs.
Okay the solution is PAs. Wait, they shouldn’t practice independently in rural areas where EM physicians won’t go.
Ok the solution is independent PAs and NPs. Nevermind, they will take EM physician jobs from EM physicians because that’s entirely possible.
Ok, let’s just keep it as is.
Honestly, it doesn’t matter what EM physicians think because they are employees without any control of their speciality. This is the appeal of FM with strong EM training because you can do private practice much more easily and supplement with ED shifts when the price is right. This is how medicine was practiced when doctors had control. Now we’re all just slaves with no business sense training our replacements.
Back to facts. It’s possible for an FM with EM fellowship training to have spent 20+ months in the ED seeing those same difficult airways. And don’t act like you didn’t do an elective to get ICU experience and a million pediatric airways. Other specialties can use elective time too. But let’s avoid inconvenient logic and return to your original argument that EM training is only possible in the vacuum that is EM residency training.
Those are all fair points. I still think the individual physician knows whether or not they are ready to practice safely. .
Leroy -
I was about to throw you a bone.
You almost have a point regarding an FP doc who does another 12-20 months in an ED under the supervision of ABEM docs. I would grant you that an FP doc who did these 12-20 months as a "fellow" in an ED that has an ACGME-approved EM residency (including all classroom didactics, peds EM shifts, ICU senior months, etc.) alongside EM residents would probably be nearing adequate training (although 20 months is almost the required 24-30 months to just complete the EM residency and be double boarded).
However, your most recent post in the anesthesiology forum (about NPs doing pre-ops) gives away your character and frequent purpose.
For everyone, else: when Leroy gets close to making a reasonable point regarding more EM training for FP docs, please do not neglect to acknowledge the greatly different learning environments (trainees, classroom diadiactics, culture, etc) in those EDs with ACGME-approved EM residencies and the EM "fellowship" year for FP docs. It has way more importance than just a Level 1 trauma center distinction. Indeed, most EM residents know that Level I status is of minimal importance compared to the rest that an EM residency has to offer.
HH
If you have the skills to stabilize someone, then what's the issue exactly? There are plenty of things pgy3s in EM have not done but may encounter in the real world. There are also FM residents (the limited ones who choose to pursue it) in unopposed programs that get a lot of intubations/lines etc.But just because you don't want to do something full time, doesn't mean you can shirk the training necessary to do that job. I can tube, sedate, block and manage a vent but that wouldn't necessarily make me qualified to be a part time-anaesthesiologist regardless of how comfortable I think I am in the OR.
Idk, maybe I'm missing something but I don't really understand how someone could be comfortable not seeking training in a job they weren't actually trained for, and why they would want to be board certified in a job they didn't train for and don't have plans on practicing full time.
Source for bad outcomes?Its almost like there was a time at some point where FPs and others did run EDs. Its also almost like the outcomes sucked and so it was decided that we needed dedicated doctors in the ED with training directed specifically at emergency medicine.
That's what happens in a lot of Canada and outcomes are identical to USA. I'm sure they don't get trauma, STEMIs, pneumothorax among other things.I’ve talked to a few applicants on the trail and it’s scary the number of people who think 3-4 months of em electives in residency is enough to get by to work in the ED safely.
I just wanted to point out that I've taken calls from outside facilities, and continue to be astonished at the lack of basic medical knowledge of some physicians. Granted, I didn't ask them if they were trained as FM, EM or children's cereal maker. . . . the lines are recorded after all.
- Don't trust anyone who says "ABPS certification" is just as good. Because it's not. It's not universally accepted, so don't rely on it.
- Equating the competency skill of the average EM graduate with the average FM graduate who did a 1 year emergency fellowship is a false equivalency.
- If you think you want to do something more advanced (work in a Level 1 trauma center, etc), either just do an EM residency or an FM/EM combined residency.
Well for starters, the EM residents where I did med school get 108 weeks in the ED. Your numbers for an FM with the fellowship are off as the handful of programs who publish their curricula are not solely spent in the ED.Not sure why you think a FM doc who spends 60-70 wks training in the ED (52 wks fellowship and their time in the ED as a FM resident) would not be good to practice EM...
You're the one who wants to change the status quo, its on you to prove that outcomes are the same.Source for bad outcomes?
Fair enough!Well for starters, the EM residents where I did med school get 108 weeks in the ED. Your numbers for an FM with the fellowship are off as the handful of programs who publish their curricula are not solely spent in the ED.
At my old residency program, you get 22 weeks of electives plus 6 weeks in the ED. The 2 EM-fellowship programs I could find that publish their rotation schedules, you end up with 34 and 36 weeks respectively. So we're talking more like ~60 weeks versus 108. So barely over half the time.
Most FM programs only have at most 1 month of ICU time. Compare that to the 8 weeks of MICU time, 4 weeks of PICU time, and 4 weeks STICU time EM residents receive.
The post you were replying to said that equating an EM graduate with an FM graduate who did 1 year of fellowship is false, and it very clearly is.
Now that said, can an FP who does everything they can to become good at emergency medicine do OK in an ED somewhere? Almost certainly. Will they be better than an EM-trained doctor? Almost certainly not.
Which would be why no other specialty has them to begin with.Fair enough!
Maybe they should create 18-month fellowship EM for FM grad who later discover they don't like the day-to-day practice of FM. In my opinion, an EM fellowship track for FM doc would make more sense than any other specialty.
If you have the skills to stabilize someone, then what's the issue exactly? There are plenty of things pgy3s in EM have not done but may encounter in the real world. There are also FM residents (the limited ones who choose to pursue it) in unopposed programs that get a lot of intubations/lines etc.
Well for starters, the EM residents where I did med school get 108 weeks in the ED. Your numbers for an FM with the fellowship are off as the handful of programs who publish their curricula are not solely spent in the ED.
At my old residency program, you get 22 weeks of electives plus 6 weeks in the ED. The 2 EM-fellowship programs I could find that publish their rotation schedules, you end up with 34 and 36 weeks respectively. So we're talking more like ~60 weeks versus 108. So barely over half the time.
Most FM programs only have at most 1 month of ICU time. Compare that to the 8 weeks of MICU time, 4 weeks of PICU time, and 4 weeks STICU time EM residents receive.
The post you were replying to said that equating an EM graduate with an FM graduate who did 1 year of fellowship is false, and it very clearly is.
Now that said, can an FP who does everything they can to become good at emergency medicine do OK in an ED somewhere? Almost certainly. Will they be better than an EM-trained doctor? Almost certainly not.
Fair enough!
Maybe they should create 18-month fellowship EM for FM grad who later discover they don't like the day-to-day practice of FM. In my opinion, an EM fellowship track for FM doc would make more sense than any other specialty.
Sigh.Problem 1) you’re comparing EM residency training to what you think is the average family medicine program. Whether or not your assumptions about FM training are true, no one is arguing that the average family doctor is better at EM than an EM physician.
Problem 2) you’re assuming the only skills used in the ED are learned in the ED. You place a premium on your 10 deliveries or whatever required for graduation learned while shadowing an OB off service and discount clearly superior OB/GYN training, c-section/high risk, etc training of FM. I’ll save you the anecdotal evidence of EM physicians treating preeclampsia like a migraine at my hospital. Preeclampsia is a life threatening emergency you know.. thankfully they were admitted to our FM service
Problem 3) you’re putting a premium on the value of off service elective time for EM residents. We’ve all done useless off service electives where we’re mostly shadowing with non faculty who could care less. In an unopposed FM program, you’re admitting and managing patients in the ICU longitudinally on all of your patients and making decisions under a FM attending that gives you much more autonomy.
I’ll give you that EM residents spend more time in the ED initially. I won’t give you that FM graduates have a magical fairy that follows them around and prevents them from ever gaining enough ED experience to practice.
Why a legit fellowship would patients in a dangerous situation? I don’t get it...If someone doesn't like the day-to-day practice of FM, the "out" should not be a fellowship that may well put you, and your patients, in a dangerous situation. It would make more sense to either switch specialties while still in residency, do a second residency, do urgent care, or do one of the other fellowships, like sports or sleep. But doing an EM fellowship with the assumption that you'll definitely always find work in whichever ER you choose is disingenuous.
Why a legit fellowship would patients in a dangerous situation? I don’t get it...
If it happens with success in the country up north, it's viable. From what I experienced and observed, FM docs (though significant ED exp) did a drastically better job of managing very sick patients with 0 (or limited) back up.Again, it's not simply about tubes and lines. Being able to identify sick people and prevent them from decompensating, resuscitating those in extremis effectively, disposition people in a timely manner while maintaining workflow is a skill that literally takes years to develop. Most FM grads don't have that skill.
This question has been asked millions of times on this forum and even ICU attendings have said that they couldn't work in an ER. Being good at resuscitation is necessary, not sufficient, for the job.
If it happens with success in the country up north, it's viable. From what I experienced and observed, FM docs (though significant ED exp) did a drastically better job of managing very sick patients with 0 (or limited) back up.
But I will agree strongly that most FMs in the US absolutely do not have that skill. We may also be disregarding talent in the equation... some residents see a procedure once, do it with competence after. Others can do it 10x and still suck. And taking care of acute patients also takes a certain mindset. Some people pick it up far quicker than others. The rest is about the medical knowledge and hands-on skills.
Yes, they don't have trauma and medically complex patients.Canada =/= USA.
Yes, they don't have trauma and medically complex patients.
Yes, they don't have trauma and medically complex patients.
we've already established that the US is fatter, with more chronic conditions, fewer PCPs to manage those conditions, more violent with more AIDS and a higher all-cause mortality rate than Canada is.
The problem is how we identify those FPsAnd the US has way more ERs with infinitely more resources & residencies etc.
Try managing an over-packed ER with a 7 hour wait time as the only physician with no CT scanner and access to a fraction of the labs/tests. Can't get an airway? Tough luck, you have to. Outside of the veryyy few academic urban centers, most ED docs are seeing and doing a lot more solo, even in large community settings. The equivalent setting in USA would have an EM residency among other residencies in the hospital. Basically an army backs you up 24/7.
So either FM residents/med students are far better trained from day 1 over there, or... FM has the capability to handle ER work. But I do agree that MOST family med residents are not trained nor equipped to handle it at all. We're talking about ones who have had an interest in it from med school and developed skills over time for it, then later improve into early attending years.
The problem is how we identify those FPs
Well basic criteria is prior ED experience.
There's also significant interest in ER and gearing all of your electives towards it. Occasionally some FM residents will do so, even longitudinally (working ER shifts all 3 years, going to the OR to intubate some mornings, etc.).
The reason we get this crossover is that there's major overlap with FM and EM, and lot of people like the idea of doing both and/or not full time ER forever. With outpatient to fall back on later.
