ERAS Pathway Improves Analgesia, Opioid Use and PONV Following Total Mastectomy
New Orleans—With surgery still the primary treatment for breast cancer, strategies to minimize acute postoperative pain have the potential for significant benefit, perhaps even preventing development of chronic pain. A research team at the University of California, San Francisco (UCSF) has moved much closer to this lofty goal. They developed an enhanced recovery after surgery (ERAS) pathway that significantly decreased opioid consumption, acute postoperative pain, and postoperative nausea and vomiting (PONV) in women undergoing total mastectomy.
“There’s a movement in anesthesia to improve patient care by implementing ERAS pathways,” said Monica Harbell, MD, assistant clinical professor of anesthesia and perioperative care at UCSF’s School of Medicine. “Nevertheless, there haven't been many enhanced recovery pathways in breast surgery. So we wanted to apply the principles of enhanced recovery in an effort to get our patients mobilized earlier, more active and involved in their care, and hopefully achieve better outcomes and greater patient satisfaction.”
The pathway calls for preoperative administration of 600 mg oral gabapentin and 1,000 mg oral acetaminophen in all patients, as well as placement of 1.5 mg transdermal scopolamine in patients aged less than 60 years with multiple risk factors for PONV. Intraoperatively, the pathway recommends total IV anesthesia, minimizes opioids,
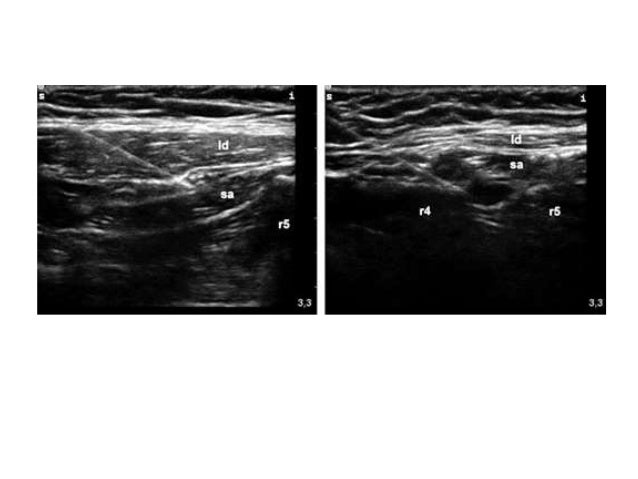
uses regional anesthesia (either Pec 1 and 2 or paravertebral blocks), and PONV prevention with 8 mg IV dexamethasone and 4 mg IV ondansetron. In the PACU, patients receive opioids, ondansetron and/or lorazepam as needed.
“And then we really encourage patients to mobilize as early as possible after surgery, to make sure we decrease risks that come with immobility, such as pneumonia and DVTs [deep venous thromboses],” Dr. Harbell said.
To help determine the efficacy of the pathway, the researchers studied 350 patients undergoing total mastectomy surgeries at UCSF Medical Center between Jan. 1, 2014 and Dec. 22, 2015. The hospital’s ERAS pathway for total mastectomy was implemented on July 1, 2015.
As Dr. Harbell and the study’s lead author Catherine Chiu, BS, reported at the 2016 annual meeting of the American Society of Regional Anesthesia and Pain Medicine (abstract 1292), 65 of the 350 participants were enrolled in the ERAS pathway; the two groups were demographically similar. After implementation of the pathway, the researchers found significant increases in many perioperative treatment parameters, including the number of patients who received preoperative acetaminophen (from 17% to 89%;
P<0.001), preoperative gabapentin (from 12% to 85%;
P<0.001), preoperative scopolamine (from 23% to 72%; P<0.001), intraoperative nerve blocks (from 19% to 85%;
P<0.001) and intraoperative total IV anesthesia (from 7% to 28%;
P<0.001).
The pathway also significantly increased perioperative time by five minutes (P=0.008), but did not change PACU recovery time.
“I think there was some initial concern that placement of a regional block would add a substantial amount of time to the procedure,” Dr. Harbell said. “But we didn’t find any difference in the length of time that it took from when you entered the operating room to the time you left, excluding surgical time. It’s nice to know that what we’re doing is not making a negative impact on the flow of the day, but at the same time is adding patient benefit.”
Median perioperative opioid consumption significantly decreased with enrollment in the ERAS pathway, from 34.2 mg IV morphine equivalents to 21.4 mg. ERAS patients also reported a one-point reduction in postoperative pain (0-10 numeric rating scale). Finally, PONV—defined as the need for administration of any antiemetic—significantly decreased with ERAS enrollment, from an incidence of 50% to 8%.
“We found that the biggest decrease in opioid consumption was actually in the PACU period,” Dr. Harbell said. “Yet it’s hard to know which intervention is adding the most in the recovery period; it’s probably the combination of everything.”
With these positive results,
Dr. Harbell was quick to recommend that other institutions consider implementing similar pathways for women undergoing total mastectomy. “I think the parts of our pathway that we highlight can definitely be instituted everywhere,” she said, “and that’s what’s nice about the pathway that we’ve developed.”
Yet success goes well beyond following steps on a flowchart. Indeed, the foundation of a healthy ERAS pathway, she explained, is interdisciplinary collaboration. “We’re very lucky in that our surgeons and other perioperative health care providers are supportive of the pathway. I think that’s partly why we’ve been successful: It’s not just anesthesiology working in isolation. You have to engage the other care members and make sure everyone has a chance to provide input. It definitely makes things run much more smoothly.”
Dr. Harbell added, “Of course, you have to figure out what works best for your institution, because what works for one group may not work for another, depending on the infrastructure and resources they have available.”
Joseph Myers, MD, associate professor of anesthesiology and chief of obstetric anesthesia at Georgetown University, in Washington, D.C., told
Anesthesiology News that Dr. Harbell has formalized a classic ERAS strategy for mastectomy patients: List potential problems, choose evidence-based solutions and then create a protocol for consistency. “Avoiding or reducing the use of opioids is difficult since their use has become so dogmatic,” he said. “But there are so many alternatives. We need to learn to trust their effectiveness.
“By involving the surgical team in the postoperative analgesic plan, with the placement of the nerve block, our combined efforts benefit the patient tremendously,” said Dr. Myers. “I find that the surgical team will gladly collaborate with us, if only we ask. It’s important that anesthesia leads the way in this regard.”
—Michael Vlessides
http://www.anesthesiologynews.com/M...ONV-Following-Total-Mastectomy/36353/ses=ogst