Can a Physician Assistant Cover your radiation clinic while you're at a satellite location within a 5 mile radius?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Can a Physician Assistant Cover your radiation clinic while you're at a satellite?
- Thread starter XRT_doc
- Start date
- Joined
- Feb 11, 2005
- Messages
- 579
- Reaction score
- 448
sure - as long as you are not treating patients.
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
I'm inquiring while patients are getting treatment. Can a Physician Assistant be there instead of the radiation oncologist while the radiation oncologist is at another facility within a 5 mile radius.
I know personally of several facilities in Texas who do this but I'm wondering about the legality of it. Some of these are major hospital institutions.
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
I'm inquiring while patients are getting treatment. Can a Physician Assistant be there instead of the radiation oncologist while the radiation oncologist is at another facility within a 5 mile radius.
I know personally of several facilities in Texas who do this but I'm wondering about the legality of it. Some of these are major hospital institutions.
6-7 figure legal settlements in multiple states (including TX) suggest it would be unwise to do so while treating Medicare/Medicaid or Tricare patients.
Hard to be "immediately available" to check an IGRT at the machine from several miles away
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Actually you can probably treat. You just can't bill CMS/tricare for services on their patientssure - as long as you are not treating patients.
6-7 figure legal settlements in multiple states (including TX) suggest it would be unwise to do so while treating Medicare/Medicaid or Tricare patients.
Hard to be "immediately available" to check an IGRT at the machine from several miles away
Well most centers now have the ability to remotely check the images. I rarely check the images on the machine, though I usually do it from my desk in my office.
But I agree the case settlements clearly make it seem like a risky endeavor to do so. I'd want to get it in writing from medicare that it's kosher before proceeding.
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Well most centers now have the ability to remotely check the images. I rarely check the images on the machine, though I usually do it from my desk in my office.
But I agree the case settlements clearly make it seem like a risky endeavor to do so. I'd want to get it in writing from medicare that it's kosher before proceeding.
Let me know when CMS does that for you
When it comes to cbct, my therapists will still come get me to check alignment before they treat
- Joined
- Feb 11, 2005
- Messages
- 579
- Reaction score
- 448
There are some exceptions for rural locations (that are negotiated with CMS) but I honestly don't know how that works or what qualifies.
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
They are called CAHs, or critical access hospitals. It's a special designation by Medicare.There are some exceptions for rural locations (that are negotiated with CMS) but I honestly don't know how that works or what qualifies.
I'm with you on that one, never have actually seen one
ABSOLUTELY ,they can if it a hospital based center. No, if it is a freestanding center.
CMS specifically included non physician provider (NPP) in the regulation. It is totally unambiguous. IT is in writing from medicare!
Hospital BASED CENTER: "Direct supervision is required for radiation therapy services provided in the hospital outpatient department. In general and per Medicare regulations, either a physician or a non-physician practitioner may directly supervise hospital outpatient therapeutic services.1 However, the supervising physician or non-physician practitioner must have within his or her State scope of practice and hospital-granted privileges the ability to perform the service or procedure that he or she supervises."
https://www.astro.org/uploadedFiles...tice/Content_Pieces/SupervisionWhitePaper.pdf
CMS specifically included non physician provider (NPP) in the regulation. It is totally unambiguous. IT is in writing from medicare!
Hospital BASED CENTER: "Direct supervision is required for radiation therapy services provided in the hospital outpatient department. In general and per Medicare regulations, either a physician or a non-physician practitioner may directly supervise hospital outpatient therapeutic services.1 However, the supervising physician or non-physician practitioner must have within his or her State scope of practice and hospital-granted privileges the ability to perform the service or procedure that he or she supervises."
https://www.astro.org/uploadedFiles...tice/Content_Pieces/SupervisionWhitePaper.pdf
Last edited:
ABSOLUTELY ,they can if it a hospital based center. No, if it is a freestanding center.
CMS specifically included non physician provider (NPP) in the regulation. It is totally unambiguous. IT is in writing from medicare!
Hospital BASED CENTER: "Direct supervision is required for radiation therapy services provided in the hospital outpatient department. In general and per Medicare regulations, either a physician or a non-physician practitioner may directly supervise hospital outpatient therapeutic services.1 However, the supervising physician or non-physician practitioner must have within his or her State scope of practice and hospital-granted privileges the ability to perform the service or procedure that he or she supervises."
https://www.astro.org/uploadedFiles...tice/Content_Pieces/SupervisionWhitePaper.pdf
Well this is clear documentation from ASTRO that it's possible to have PA cover in hospital based setting.
- Joined
- Mar 20, 2013
- Messages
- 1,909
- Reaction score
- 3,496
ABSOLUTELY ,they can if it a hospital based center. No, if it is a freestanding center.
CMS specifically included non physician provider (NPP) in the regulation. It is totally unambiguous. IT is in writing from medicare!
Hospital BASED CENTER: "Direct supervision is required for radiation therapy services provided in the hospital outpatient department. In general and per Medicare regulations, either a physician or a non-physician practitioner may directly supervise hospital outpatient therapeutic services.1 However, the supervising physician or non-physician practitioner must have within his or her State scope of practice and hospital-granted privileges the ability to perform the service or procedure that he or she supervises."
https://www.astro.org/uploadedFiles...tice/Content_Pieces/SupervisionWhitePaper.pdf
This new 2018 update from ASTRO does suggest a non-physician practitioner may be included.
However, later on the article it does state this:
"The supervisory responsibility is more than the capacity to respond to an emergency. It is ASTRO’s opinion that a board-certified/board-eligible Radiation Oncologist is the clinically appropriate physician to supervise radiation treatments."
I think *for now,* if all your ducks are in a row and you have a well documented scope of practice (ie can cover routine treatments, but no SBRT, CT sims, HDR, etc) for a PA/NP in writing with a massive paper trail including having the med exec committee of the hospital approve it (CMS loves to pawn off ambiguity to the discretion of the hospital)...then it may be OK. THe risk you run is getting into a whistleblower lawsuit, which are becoming common now when therapists blow the whistle and end up getting a cut (like 25%) of all medicare money that is recuperated as part of a suit/investigation.
This new 2018 update from ASTRO does suggest a non-physician practitioner may be included.
However, later on the article it does state this:
"The supervisory responsibility is more than the capacity to respond to an emergency. It is ASTRO’s opinion that a board-certified/board-eligible Radiation Oncologist is the clinically appropriate physician to supervise radiation treatments."
I think *for now,* if all your ducks are in a row and you have a well documented scope of practice (ie can cover routine treatments, but no SBRT, CT sims, HDR, etc) for a PA/NP in writing with a massive paper trail including having the med exec committee of the hospital approve it (CMS loves to pawn off ambiguity to the discretion of the hospital)...then it may be OK. THe risk you run is getting into a whistleblower lawsuit, which are becoming common now when therapists blow the whistle and end up getting a cut (like 25%) of all medicare money that is recuperated as part of a suit/investigation.
For hospital centers, the cms/medicare language has been the same for at least 5 years and has always included (npp) non-physician provider. ASTRO is just quoting it. Personally, I dont have an NPP, but I see this as an area that could impact the job market.
This new 2018 update from ASTRO does suggest a non-physician practitioner may be included.
However, later on the article it does state this:
"The supervisory responsibility is more than the capacity to respond to an emergency. It is ASTRO’s opinion that a board-certified/board-eligible Radiation Oncologist is the clinically appropriate physician to supervise radiation treatments."
I think *for now,* if all your ducks are in a row and you have a well documented scope of practice (ie can cover routine treatments, but no SBRT, CT sims, HDR, etc) for a PA/NP in writing with a massive paper trail including having the med exec committee of the hospital approve it (CMS loves to pawn off ambiguity to the discretion of the hospital)...then it may be OK. THe risk you run is getting into a whistleblower lawsuit, which are becoming common now when therapists blow the whistle and end up getting a cut (like 25%) of all medicare money that is recuperated as part of a suit/investigation.
I'm not sure why a what the whistleblower will whistle about since documentation says its allowed. Of course the scope of the PA will be only to be the "body" present. The images, weeklysees, and any HDR will be done by the radiation oncologist.
For hospital centers, the cms/medicare language has been the same for at least 5 years and has always included (npp) non-physician provider. ASTRO is just quoting it. Personally, I dont have an NPP, but I see this as an area that could impact the job market.
Let's keep this thread on topic. I don't want this to become a thread on the preservation of the job market which there are plenty of threads for.
The NPP would need to be trained in radiation oncology with documented work history or competencies to get privileges at most hospitals.
You couldnt have the cardiac pa supervising this while they do inpts rounds.
You couldnt have the cardiac pa supervising this while they do inpts rounds.
- Joined
- Mar 20, 2013
- Messages
- 1,909
- Reaction score
- 3,496
I'm not sure why a what the whistleblower will whistle about since documentation says its allowed. Of course the scope of the PA will be only to be the "body" present. The images, weeklysees, and any HDR will be done by the radiation oncologist.
Images has been the key hang up we've dealt with. Can you bill your professional CBCT code by checking that image remotely but not being personally present to supervise? If you are billing it under your NPI number but an on site NP is the one actually supervising it, is that still OK?
I know for a fact this goes on at multiple places (at least it was five years ago), including academic centers....but our risk managers at the hospital even with this CMS guideline and prior astro statements have been unwilling to let us use an NP for routine coverage.
Images has been the key hang up we've dealt with. Can you bill your professional CBCT code by checking that image remotely but not being personally present to supervise? If you are billing it under your NPI number but an on site NP is the one actually supervising it, is that still OK?
I know for a fact this goes on at multiple places (at least it was five years ago), including academic centers....but our risk managers at the hospital even with this CMS guideline and prior astro statements have been unwilling to let us use an NP for routine coverage.
Though the current CMS guideline and ASTRO statement clearly states that its allowed. I believe the CBCT should be approved by the radonc and I don't see how it's any different for it to be approved from a remote office than an office in the facility since the CBCT is usually approved at the end of the day when the patient is gone.
- Joined
- Mar 20, 2013
- Messages
- 1,909
- Reaction score
- 3,496
Though the current CMS guideline and ASTRO statement clearly states that its allowed. I believe the CBCT should be approved by the radonc and I don't see how it's any different for it to be approved from a remote office than an office in the facility since the CBCT is usually approved at the end of the day when the patient is gone.
Agreed.
I have stubborn administrators/risk management though that can't seem to get this. However, what about the scenario where the CBCT looks pretty off and the therapists need assistance. This happens at least once a day at my clinic. Can the NP assist with that if trained appropriately?
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
.1 However, the supervising physician or non-physician practitioner must have within his or her State scope of practice and hospital-granted privileges the ability to perform the service or procedure that he or she
Though the current CMS guideline and ASTRO statement clearly states that its allowed. I believe the CBCT should be approved by the radonc and I don't see how it's any different for it to be approved from a remote office than an office in the facility since the CBCT is usually approved at the end of the day when the patient is gone.
Unless the billing provider is able to "immediately" provide assistance in "furnishing the procedure", Medicare is going to have a problem with it imo.
That language is straight from cms guidelines. Again, you might be ok if the PA is trained in igrt and is the one who is able to line up a cbct (again only in a hospital setting).
If the physician is remotely checking a cbct (and billing for it) but isn't able to adjust it at the machine, I personally think that's running afoul of cms guidelines. Again, it's always best to seek legal counsel when issues like this come up
Last edited:
D
deleted18755
Can a Physician Assistant Cover your radiation clinic while you're at a satellite location within a 5 mile radius?
Just curious and sorry if it's a bit off topic but how/why do you have two locations within a 5 mile radius? Are you in the middle of Manhattan (in which case from what I understand it could take you an hour to travel 5 miles so that's a big deal) or in "normal" location where you could travel 5 miles in <10-15 minutes (and presumably so too could your patients, so why a "satellite"?).
Having two centers that close seems so odd but what do I know?
Just curious and sorry if it's a bit off topic but how/why do you have two locations within a 5 mile radius? Are you in the middle of Manhattan (in which case from what I understand it could take you an hour to travel 5 miles so that's a big deal) or in "normal" location where you could travel 5 miles in <10-15 minutes (and presumably so too could your patients, so why a "satellite"?).
Having two centers that close seems so odd but what do I know?
I agree it doesn't make a whole lot of sense to keep two centers within 5 minutes of each other (which they are).
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Happens when another vault is needed and the existing facility can't accommodate... esp if there are competing hospital systems 5 miles apart with different referral networks.Just curious and sorry if it's a bit off topic but how/why do you have two locations within a 5 mile radius? Are you in the middle of Manhattan (in which case from what I understand it could take you an hour to travel 5 miles so that's a big deal) or in "normal" location where you could travel 5 miles in <10-15 minutes (and presumably so too could your patients, so why a "satellite"?).
Having two centers that close seems so odd but what do I know?
Happened in my practice, prior to the current era of physician supervision requirements
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
Literally thousands of CT images are checked remotely every day without the checking physician (radiologist) being personally present to supervise the actual CT, yes? (I mention this because in the CMS benefit manual, radiation oncology and radiology are in the same section/chapter and CMS calls the radiation oncologists "radiologists" lots of times.) In short, it's clear just based on the written law that advanced practice practitioners can provide direct supervision of diagnostic and therapeutic procedures in the hospital. But, even when the law is clear, in our specialty confusion over a great many things still abounds. What's surprising is: 1) Why the hospitals haven't used the plainly written law to add to their bottom line (i.e. "spread" a rad onc MD across a few hospitals--why hire multiple rad oncs when just 1 and a few NPs will do?), and 2) why we in radiation oncology are so confused about the in-hospital issue (but our ACR radiology brethren seem not to be). EDIT: I will also add that a few years ago I obtained a written, well-detailed opinion from very well known rad onc who sits on many Medicare committees, helped draft rules, etc., explaining that it can be a non-rad onc MD the hospital appoints to supervise when the rad onc is out, or an NP or PA. Regardless of his opinion though, no one I showed it to believed it!Can you bill your professional CBCT code by checking that image remotely but not being personally present to supervise?
Last edited:
D
deleted18755
Happens when another vault is needed and the existing facility can't accommodate... esp if there are competing hospital systems 5 miles apart with different referral networks.
Happened in my practice, prior to the current era of physician supervision requirements
Oh yeah that makes sense with the cost of a new vault (but then again you probably don't need double but certainly have to pay extra staff . . . and an MD apparently.)
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
EDIT: I will also add that a few years ago I obtained a written, well-detailed opinion from very well known rad onc who sits on many Medicare committees, helped draft rules, etc., explaining that it can be a non-rad onc MD the hospital appoints to supervise when the rad onc is out, or an NP or PA. Regardless of his opinion though, no one I showed it to believed it!
Despite all of that, we still see multi-million dollar settlements happening in both freestanding and hospital-based practices regarding physician supervision issues.
Why is that happening? (Especially in the hospital-based practices)
- Joined
- Mar 20, 2013
- Messages
- 1,909
- Reaction score
- 3,496
Literally thousands of CT images are checked remotely every day without the checking physician (radiologist) being personally present to supervise the actual CT, yes? (I mention this because in the CMS benefit manual, radiation oncology and radiology are in the same section/chapter and CMS calls the radiation oncologists "radiologists" lots of times.) In short, it's clear just based on the written law that advanced practice practitioners can provide direct supervision of diagnostic and therapeutic procedures in the hospital. But, even when the law is clear, in our specialty confusion over a great many things still abounds. What's surprising is: 1) Why the hospitals haven't used the plainly written law to add to their bottom line (i.e. "spread" a rad onc MD across a few hospitals--why hire multiple rad oncs when just 1 and a few NPs will do?), and 2) why we in radiation oncology are so confused about the in-hospital issue (but our ACR radiology brethren seem not to be). EDIT: I will also add that a few years ago I obtained a written, well-detailed opinion from very well known rad onc who sits on many Medicare committees, helped draft rules, etc., explaining that it can be a non-rad onc MD the hospital appoints to supervise when the rad onc is out, or an NP or PA. Regardless of his opinion though, no one I showed it to believed it!
I don't disagree with you, but this is the bottom line question that always gets asked, and I'm not sure I've seen congruent answers from all people involved:
So if you are checking a CBCT remotely and billing a CBCT from a professional standpoint (CPT 77014-26), do you bill it under the NP there able to assist with the procedure, or do you bill it under the physician checking it remotely?
- Joined
- Apr 16, 2004
- Messages
- 4,659
- Reaction score
- 5,070
Why is that happening? (Especially in the hospital-based practices)
Top reasons are disgruntled employees and the whistleblowers fee provided by CMS
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Regardless of the reasons, these cases are very real and settled for obscene amounts of money.Top reasons are disgruntled employees and the whistleblowers fee provided by CMS
I've seen private practices lose their PSAs over it in hospital-based practices and the new RO hires are then employed by the hospital where they obviously have more control over them in terms of physical presence requirements.
Personally, I would be cautious in this regard if I was a hospital-based PP RO trying to have extenders cover me for igrt at remote sites
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
Idk. They didn't fight? The freestanding ones have been far more common than hospital. Every single time I've had an "expert" look at the hospital situation, they've said it can be any MD, or NP or PA. (EDIT: the CBCT code is a 77xxx code, ie a radiology code... heck, even the family practice docs get to bill 77xxx codes right?) Every time this is brought to hospital admin, they disagree. As do hospital attorneys. So it's a dilemma. And oft times it's just way easier to settle than fight; fight has a low upside, potentially terrible downside.Despite all of that, we still see multi-million dollar settlements happening in both freestanding and hospital-based practices regarding physician supervision issues.
Why is that happening? (Especially in the hospital-based practices)
Isn't the procedure a 77014-TC (which you can never bill for as MD in hospital), and what you do re: "the checking" the -26 charge? The -26 is not charged until the moment you as MD check the film (btw Medicare officially calls the 77014-26 "supervision undefined" level 9 in the charge list, and "direct" level 2 for 77014-TC). In other words, the NP did nothing billable just by being there. And even if there's a question about setup etc., that activity in and of itself has no charge either (by the MD or the hospital). I have never used an NP or PA, but even when there's a radiology PA at the hospital e.g., or like no radiologist or PA around at all when CTs are done at night in a smaller hospital, the radiologists or night hawks bill full professional for reading the CTs, MRIs, X-rays (I am told).So if you are checking a CBCT remotely and billing a CBCT from a professional standpoint (CPT 77014-26), do you bill it under the NP there able to assist with the procedure, or do you bill it under the physician checking it remotely?
At the end of the day, I bet we all know a few hospital practices (and some academic ones at that) that occasionally rely on NPs or PAs. Also, somewhat unequal protection under the law-ish, chemo can be given in freestanding centers with no MD (just NP e.g.) present at all, making the whole oncology situation really... unclear.
Last edited:
Unless the billing provider is able to "immediately" provide assistance in "furnishing the procedure", Medicare is going to have a problem with it imo.
That language is straight from cms guidelines. Again, you might be ok if the PA is trained in igrt and is the one who is able to line up a cbct (again only in a hospital setting).
If the physician is remotely checking a cbct (and billing for it) but isn't able to adjust it at the machine, I personally think that's running afoul of cms guidelines. Again, it's always best to seek legal counsel when issues like this come up
I have previously worked in large academic centers that follow regulations to a T. When igrt is performed at a satellite on one of my pts on a day that I am at the main campus, I review it remotely by the end of the day and it is billed under my name, even though there is another physician present. This is how most large hospital systems function. The bill is generated when the doc reviews the image. Everyone would be out of compliance...
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
We have whoever is physically present review and bill for the igrt that day, again this is in the freestanding setting.I have previously worked in large academic centers that follow regulations to a T. When igrt is performed at a satellite on day I am at the main campus, I review it remotely by the end of the day and it is billed under my name, even though there is a different physician present. This is how most large hospital systems function. Why does the billing provider have to be present at the time of the imaging. The bill is generated when he reviews the image. Everyone would be out of compliance...
It's the same with our MO. Whoever supervises chemo has that billing submitted under their name.
Personally, I've heard cms wants whoever is physically there to be the one it is billed under, but I don't have a reference handily available to substantiate that
Last edited:
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
I can not find the primary source right now (and perhaps who cares lol) but Carl Bogardus came out and said the MD who checks the CBCT does not have to be there (as long as some MD was there) when the CBCT was done.I have previously worked in large academic centers that follow regulations to a T. When igrt is performed at a satellite on one of my pts on a day that I am at the main campus, I review it remotely by the end of the day and it is billed under my name, even though there is a different physician present. This is how most large hospital systems function. The bill is generated when he reviews the image. Everyone would be out of compliance...
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Right nearby....
Adventist Health System to Pay $5.4 Million to Resolve False Claims Act Allegations
Florida Doctors, Hospitals and Clinics to Pay $3.5 Million to Settle Allegations of Improper Medicare, Medicaid and TRICARE Billing
Seems like a lot of money at stake to settle vs hiring a legal team for even half of that.
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
The time in which one lives plays a role too. During the Obama era, rad onc really got targeted and a bunch of new 20-something lawyers came to the DOJ with their hair on fire, replacing an old guard. Rad onc false claims were essentially unheard of in the Bush era. Pendulums swing. I wouldn't rely on that... but it's interesting to note.Right nearby....
Adventist Health System to Pay $5.4 Million to Resolve False Claims Act Allegations
Florida Doctors, Hospitals and Clinics to Pay $3.5 Million to Settle Allegations of Improper Medicare, Medicaid and TRICARE Billing
Seems like a lot of money at stake to settle vs hiring a legal team for even half of that.
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Fair points. Interesting memo from the doj oigThe time in which one lives plays a role too. During the Obama era, rad onc really got targeted and a bunch of new 20-something lawyers came to the DOJ with their hair on fire, replacing an old guard. Rad onc false claims were essentially unheard of in the Bush era. Pendulums swing. I wouldn't rely on that... but it's interesting to note.
- Joined
- Jul 6, 2004
- Messages
- 1,977
- Reaction score
- 563
I’m sure this has been answered in previous threads but why is there this ambiguous wording for the hospital based systems. They say that the non-physician practitioner must have it within the state scope of practice and hospital granted privliges the ability to perform the service or procedure that he or she supervises. So it’s pretty easy that it means the NP can’t superivse a HDR treatment or a SBRT which requires cone beam approval. But if you’re starting the day with treating prostataes for example EBRT or Palliatives early in the am is NP coverage on its own ok then?
Last edited:
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
Can the NP check kV igrt and port films? Or electron setups?I’m sure this has been answered in previous threads but why is there this ambiguous wording for the hospital based systems. They say that the non-physician practitioner must have it within the state scope of practice and hospital granted privliges the ability to perform the service or procedure that he or she supervises. So it’s pretty easy that it means the NP can’t superivse a HDR treatment or a SBRT which requires cone beam approval. But if you’re starting the day with treating prostataes for example EBRT or Palliatives early in the am is NP coverage on its own ok then?
If so, and credentialed/qualified (in the eyes of CMS and your hospital credentials committee) to do so, I would think that would be ok in a hospital-based setting. I would probably make sure you've got documentation of all of that, obviously.
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
I may be wrong... but checking or reading films is not a procedure. It's the incident-to, technical stuff we're (and the federal code) talking about NPs and PAs supervising. That is to say, when a radiologist reads a CT it's not a procedure per se. I don't think any NPs or PAs in America are "reading" the IGRT films and billing the professional at the 85% reduced rate. The MD will read the IGRT films at the end of the day long after the IGRT technical component (procedure proper) itself was done. The IGRT in SBRT is not a billable thing. The SBRT is a unique treatment in that it has a professional code. Any professional code billed would always imply/require the personal input of a physician, i.e., like a consult charge, or an operative code, etc. So we may be conflating two things: procedures/diagnostics that techs do, and MD professional things (like the professional part of an IMRT plan, weekly tx management, etc.).Can the NP check kV igrt and port films?
Last edited:
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
But isn't that CMS billing of the technical component contingent upon following the supervision guidelines? That's the crux of the issue. CMS has explicitly stated that IGRT must be supervised by someone who is "immediately available" to "assist in furnishing" the procedure. Ergo, you may be correct, but if you don't have someone who is qualified to supervise IGRT at the time the service is delivered, I believe CMS can claw that back from you, regardless of the freestanding vs hospital location.I may be wrong... but checking or reading films is not a procedure. It's the incident-to, technical stuff we're (and the federal code) talking about NPs and PAs supervising. That is to say, when a radiologist reads a CT it's not a procedure per se. I don't think any NPs or PAs in America are "reading" the IGRT films and billing the professional at the 85% reduced rate. The MD will read the IGRT films at the end of the day long after the IGRT technical component (procedure proper) itself was done. The IGRT in SBRT is not a billable thing. The SBRT is a unique treatment in that it has a professional code. Any professional code billed would always imply/require the personal input of a physician, i.e., like a consult charge, or an operative code, etc. So we may be conflating two things: procedures/diagnostics that techs do, and MD professional things (like the professional part of an IMRT plan, weekly tx management, etc.).
Cant remember where i found this, but i did at some point come across a document (possibly an astro or cms billing opinion) which basically said the doc needed to be personally present to bill even just the professional portion of igrt. There was language in the document about a physician being able to "immediately assist." I was actually working at an "open" hospital department at the time with multiple independent rad oncs billing under different tax ids, so there was always a rad onc present to bill technical. Nonetheless, I stopped billing the prof component of igrt on the days i wasnt present.
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
Techs do CT scans in radiology. The radiologist MDs may not be present in the hospital when they're done. Supervision is one thing; I don't think CMS expects techs or advance practitioners to be able to actually read the CTs. IMHO. Being "qualified" to supervise IGRT should take a 30 minute debriefing... again, IMHO. ("If the tech is uncomfortable with the auto-match, and can not satisfactorily manually match, the NP or PA is qualified to 'break' the patient for the day until the MD can assess. Alternatively, the treatment can be temporarily halted until the MD can be contacted so that treatment can resume that day. NPs or PAs are qualified to supervise IGRT if the technologists are happy with the matches and never contact the PA or NP with questions; if there are no questions, IGRT is properly supervised by an NP or PA.") Now--it really is my opinion, 'cause you can take it the other way and say the only person who can "assist in furnishing" IGRT or external beam therapy etc etc is a radiation oncologist, rendering CMS' opinion(s) that PAs/NPs can supervise a waste of words and/or a trap. Perhaps it is a trap! Future resident, do not become...CMS has explicitly stated that IGRT must be supervised by someone who is "immediately available" to "assist in furnishing" the procedure. Ergo, you may be correct, but if you don't have someone who is qualified to supervise IGRT at the time the service is delivered
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
A diagnostic CT =/= a delivery of a dose of therapeutic radiation. The igrt helps target that dose more accurately.Techs do CT scans in radiology. The radiologist MDs may not be present in the hospital when they're done.
You might have a point if the diagnostic CT has a supervision requirement on the technical side. I don't know the answer to that. Then again, this CMS definition of being able to provide assistance during igrt comes up again, which is not an issue when doing a diagnostic study
Perhaps it is a trap! Future resident, do not become...
Yup. The real question is whether whatever you choose to do will be defensible during a deposition with the doj/oig after someone blows the whistle. Pendulums swing back and qui tam lawsuits may pick up again
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
Again, if I am not mistaken, I think 77014 falls in the radiologic guidance/diagnostic range of CPT codes. (We haven't even mentioned in hospital, you can't bill the 77014-TC with IMRT anyways, and a lot of patients are IMRT obv., thus in those cases there is nothing billable for NP/PA to supervise even though "IGRT" being done.)
EDIT: BTW, **all* diagnostic procedures (technical -TC) which have CPT codes have some level of CMS-assigned supervision requirement (either 1=general, 2=direct, 3=personal, and there are other weird ones too). Interestingly all 77xxx rad onc ones which are non-technical have supervision level "9," undefined.
And yet again, I think we all agree that while the techs are delivering the dose, the NP/PA can supervise. "Our" stumbling block is not the purely/always technical charge of tx delivery.The igrt helps target that dose more accurately.
EDIT: BTW, **all* diagnostic procedures (technical -TC) which have CPT codes have some level of CMS-assigned supervision requirement (either 1=general, 2=direct, 3=personal, and there are other weird ones too). Interestingly all 77xxx rad onc ones which are non-technical have supervision level "9," undefined.
Last edited:
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
Take all this for what it's worth. Informational only!A diagnostic CT =/= a delivery of a dose of therapeutic radiation. ... The real question is whether whatever you choose to do will be defensible during a deposition with the doj/oig after someone blows the whistle. Pendulums swing back and qui tam lawsuits may pick up again
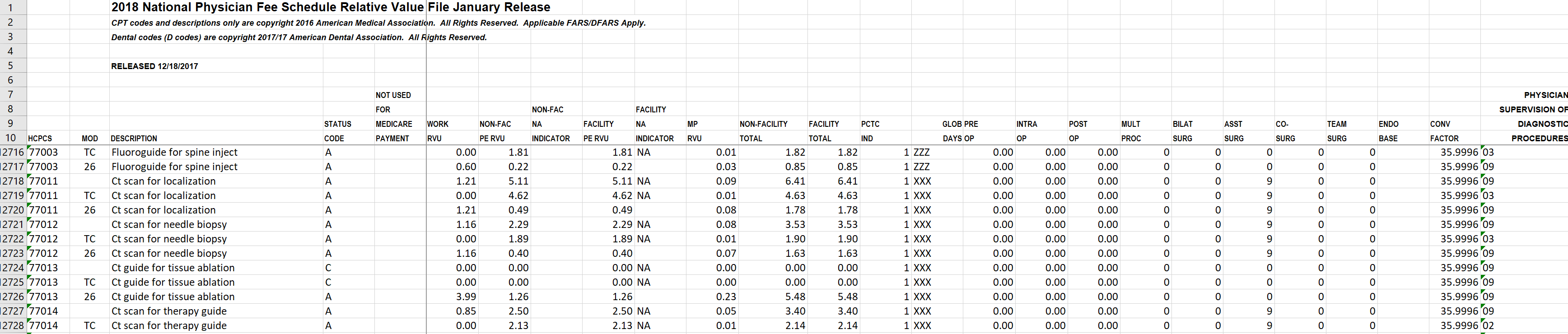
From Medicare website (see last column of spreadsheet): 77014 supervision level 9 (all global codes get a "9" as global is always assumed direct), 77014-TC is "2" and 77014-26 is "9." Per CMS manual:
Physician Supervision of Diagnostic Procedures
01 = Procedure must be performed under the general supervision of a physician.
02 = Procedure must be performed under the direct supervision of a physician.
03 = Procedure must be performed under the personal supervision of a physician.
...
09 = Concept does not apply.
Glaringly, every single 77xxx rad onc code, whether global or TC or -26, has a "9" level (again see last column), even the SBRT CPT codes. There is one code, and one code only, to which Medicare has given a "02" level and which rad oncs use: 77014-TC. Thus, and per its placement in the CPT list, it must be a diagnostic procedure... per CMS.
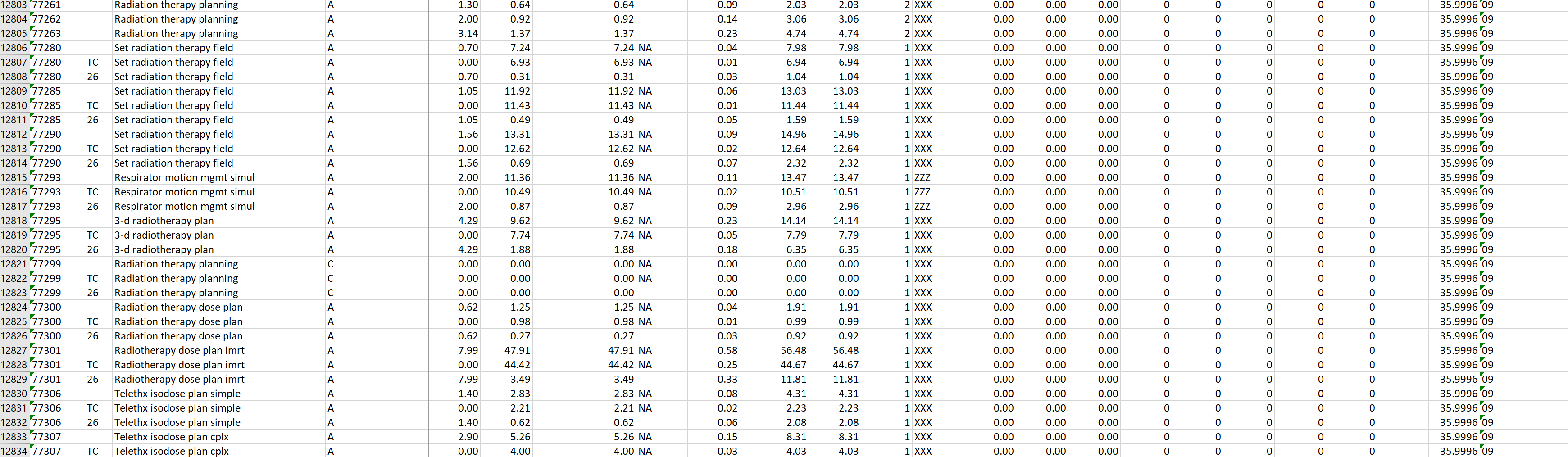
- Joined
- Sep 20, 2004
- Messages
- 11,720
- Reaction score
- 11,806
TC cbct code requires direct supervision
- Joined
- Oct 4, 2017
- Messages
- 5,013
- Reaction score
- 9,778
Cant remember where i found this, but i did at some point come across a document (possibly an astro or cms billing opinion) which basically said the doc needed to be personally present to bill even just the professional portion of igrt. There was language in the document about a physician being able to "immediately assist." I was actually working at an "open" hospital department at the time with multiple independent rad oncs billing under different tax ids, so there was always a rad onc present to bill technical. Nonetheless, I stopped billing the prof component of igrt on the days i wasnt present.
Nothing like that exists in any CMS guidance that treating doc has to be present. Could be a np/pa or another doc- someone available to step in and help (in hospital setting)
I dont believe government/DOJ is laying a trap here- I think you have to be a conspiracy theorist to believe that. They go to the effort of stating a qualifed NP/PA can supervise delivery of radiation and IGRT is integral to that delivery for many/most patients.
Last edited:
Nothing like that exists in any CMS guidance that treating doc has to be present. Could be a np/pa or another doc- someone available to step in and help (in hospital setting)
I dont believe government/DOJ is laying a trap here- I think you have to be a conspiracy theorist to believe that. They go to the effort of stating a qualifed NP/PA can supervise delivery of radiation and IGRT is integral to that delivery for many/most patients.
There are various billing issues at play here, not just supervision. An NP can supervise delivery of radiation and IGRT in a hospital, and the hospital can bill a technical component claim. No problem. However, who are you billing the professional claim under--the NP who was present while the IGRT was performed or the Rad Onc? Let's say you're billing under the rad onc, but the NP was called in on a few cases to help with the set up. Would you bill just those patients under the NP and the rest under the Rad Onc? Things can get tricky.
I wish I could find this darn guidance article I pulled up years ago. I changed my practice and gave up a significant amount of revenue on IGRT professional chargs because of it. The gist of the article was that physical presence and the ability to step in when necessary for IGRT is an inherent part of the professional component of the charge, not just the technical.
For what it's worth--I've read other papers and have spoken to other billing companies who have said bill the tech component under the doc who is present that day and the prof under whoever signs it, regardless of whether they are on site or not. I personally had too much to lose to take a chance and opted to forego billing the charge on days I wasn't present.
Last edited:
Similar threads
- Replies
- 45
- Views
- 3K
