This is a really interesting discussion. The question we are trying to answer is whether regular serologic testing for celiac disease is helpful. There are several ways to look at this.
The first is theoretical -- does it make scientific sense that this would be helpful? In general, testing autoatibodies for levels in autoimmune syndromes is not helpful. RA and SLE, the two "classic" autoimmune diseases are good examples. Although RF/anti-CCP and ANA/Anti-dsDNA might be helpful in diagnosis, they are not helpful to follow disease activity. The example above of CRP for IBD is not relevant - CRP is not an autoantibody and is a direct measure of disease activity. But TTG is celiac is notably different than RF -- we assume RF (and certainly anti-dsDNA) are antibodies to naturally present antigens in the body. TTG on the other hand is an antibody to an external antigen. If that antigen is removed, one would expect that TTG levels would fall, much like antibody titers fall after vaccinations over time. Hence, it does make some theoretical sense that TTG might behave differently than other autoantibodies and might track with disease activity.
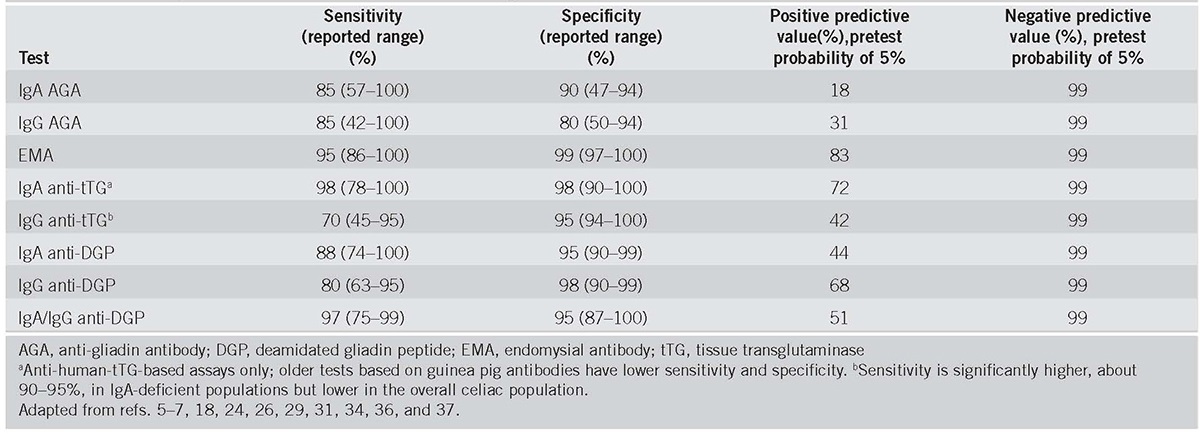
The second is practical -- do we have evidence that TTG (or other) antibodies track with disease activity? There is one study with 2000+ patients that suggests that it does:
Five year time course of celiac disease serology during gluten free diet: results of a community based "CD-Watch" program - PubMed (nih.gov) But looking at the study closely, it's not so clear. A small group of patients who were very non-compliant with the diet had persistently elevated TTG levels. Those who were better at the diet had a lower rate of TTG positivity, but because there so many more of them they make up the bulk of the positives. And what happens to these patients -- do they have an increased risk of bad outcomes? -- is unclear. There are studies in children showing that TTG levels don't match biopsy findings. So it's very tempting to think that following TTG levels might be helpful, but we have no clear evidence of such.
The third is legal / guidelines. Many GI orgs have published guidelines which suggest following antibody titers. They quote these same studies, and then recommend testing. Sadly, often in cases like this the person pushing for the tests is the one that developed the test and has a patent on it, hence generates income from the recommendation. I have no idea if that's the case here. This becomes hard to defend against in court -- how could you be smarter than the GI experts whom are publishing this? Yet their recommendations seem flawed. Suggesting that "it can't hurt" isn't true -- a patient with negative symptoms but a positive antibody is going to get more testing, if that testing shows they have active disease then they have been helped, but if nothing is found then they have been harmed by additional testing.
Like many other areas of medicine, the guidelines and evidence are a bit of a mess. Given how long we've had TTG testing, one would think that there might be long term follow up data on whether these patients with persistently elevated TTG are actually at higher risk of bad outcomes or not.