- Joined
- Oct 10, 2011
- Messages
- 8,607
- Reaction score
- 10,654
In the interest of discussing some topics that are things besides the job market and optimism/pessimism, based on a (IMO) good suggestion from an SDN user, I'm going to start a series of threads on general diagnoses and encourage people to discuss how these are managed clinically in your practice/residency/dreams, whatever. Judicious (not 80 links, but like 1-5) use of studies when relevant to the point at hand are encouraged but not mandatory.
If you have other ideas in this vein I'm open to other people starting threads as well. And so help me God, if I see a single post about the job market or other off-topic nonsense without any significant corollary to the topic in question in here I'm warning/deleting. For example, saying "We do long-course chemoRT b/c it pays better in the current era but we may see more SCRT with 5Gy x 5 in the future" is allowed.
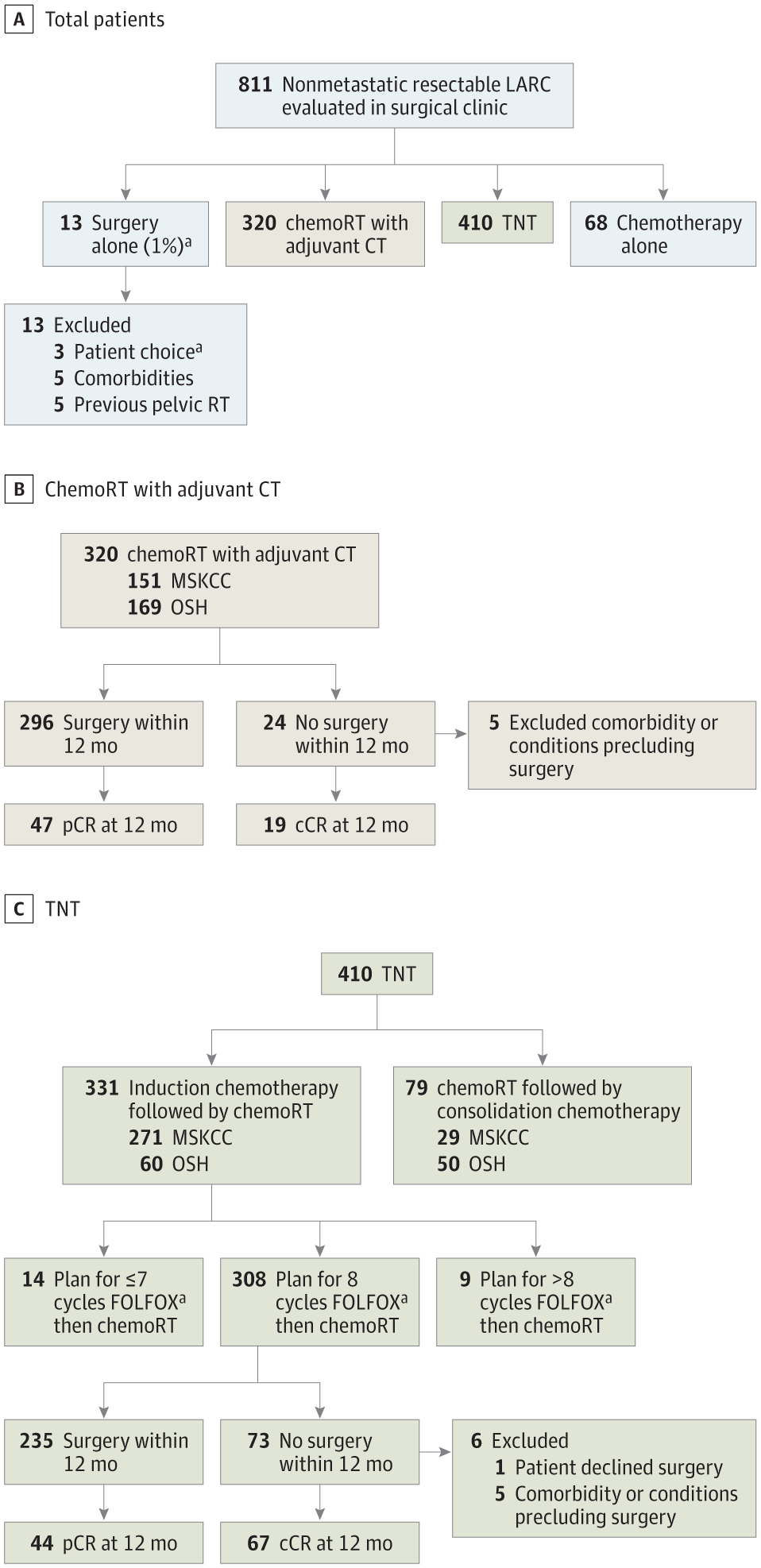
OK, so let's talk about LARC.
How are folks managing this? Everybody getting MRI, ERUS, or both?
I imagine most are doing RT in some way. Short-Course or Long-Course? What dose? Boost volume? What chemo? Does this change based on whether patient needs LAR or APR?
Are all patients getting surgery? Anybody have a robust watchful waiting process? If so, how are those patients surveilled? How do you think it works out for those patients?
What about chemotherapy? After surgery? Before surgery? If before surgery (total neoadjuvant therapy) how are you sequencing?
Anybody doing CRT followed by transanal excision?
If you have other ideas in this vein I'm open to other people starting threads as well. And so help me God, if I see a single post about the job market or other off-topic nonsense without any significant corollary to the topic in question in here I'm warning/deleting. For example, saying "We do long-course chemoRT b/c it pays better in the current era but we may see more SCRT with 5Gy x 5 in the future" is allowed.
OK, so let's talk about LARC.
How are folks managing this? Everybody getting MRI, ERUS, or both?
I imagine most are doing RT in some way. Short-Course or Long-Course? What dose? Boost volume? What chemo? Does this change based on whether patient needs LAR or APR?
Are all patients getting surgery? Anybody have a robust watchful waiting process? If so, how are those patients surveilled? How do you think it works out for those patients?
What about chemotherapy? After surgery? Before surgery? If before surgery (total neoadjuvant therapy) how are you sequencing?
Anybody doing CRT followed by transanal excision?