- Joined
- Jun 6, 2002
- Messages
- 13,869
- Reaction score
- 4,420
On the plus side, now that he's an inpatient he won't get a Press Ganey survey...
He was discharged on the first visit, so yes, he will get a Press-Ganey survey.
On the plus side, now that he's an inpatient he won't get a Press Ganey survey...
Honestly, this forum truly amazes and baffles me at times. Do you actually think this?Will state again: I would 100% not miss this diagnosis.
Its a mistake to not ask viral syndrome patients a travel history, but I rarely ask in honestly.
But since I'm not the one screening them, I'm assuming they came pre screened.
I hear ya, I use the same (and I use epic). it's a mesmerizing maze like a scene out of " the shining". wonder what they have in dallas? reverse lottery, talk about rubbing off a scratch off card and getting 4 middle fingers back at youThe EHR's are terrible. Right now looking at my CERNER tab, there are 20 tabs on the left. RN assesment has 20 more tabs. No one looks at all those tabs (if you do, you'd be looking for a new job at our place.)
What is the DDx for flu-like illness in an african patient? Viral syndrome, flu, pna, malaria, yellow fever, gastroenteritis, dengue....Tb, HIV...typhoid...hell Ebola has to be down there somewhere next to River sickness in your differential. We didn't have an Ebola policy until yesterday. To piece togehter a story from media reports (many of which are contridictory) is just asinine.
I agree with Birdstrike--you shouldn't throw stones when you work in a glass house. To the person who would have "100% not missed this diagnosis"...guess what, I 100% guarantee you have missed a diagnosis before, and will in the future. You have no idea how busy it was in the ED, maybe the Doc had 12 other patients, a STemi, a code, the waiting room had 20 in it and just got 4 new people when he saw CC of fever in a black guy who had an accent...maybe he didn't have a fever...maybe he doesn't have an accent...maybe he couldn't understand him..maybe (probably) his VS's looked fine. This is a sentinel, Black swan event.
Fortunately, we are all not lucky to have not been so unlucky to have seen the first Ebola patient ever diagnosed in the US. Now we know what not to do and what to ask for, even though it's got to be like a 1:10000000 chance anyone here will diagnose ebola. You cannot say "I would have done this" because everything is obvious in retrospect...so have some sympathy for the ER Doc who won the reverse-lottery from hell and have an ounce of humbleness, lest the ER gods hear you and take their vengence out on your hubris
i agree the nursing assessments are legal and will save you one day. communication is always the #1 problem between health care providers. it's when they document a ton of stuff and not tell you, that's the problemAlthough I feel that this could probably blow up on me, I will say that professional RNs are educated and required by their nurse practice act and SOP to obtain admission assessments and histories. The RN, if she/he is one, is responsible to not only take such relevant information down and be aware of the implications of it, he or she is also required to report these findings directly, by face or by phone, with a physician supervising the medical care of the patient and to in fact indicate that she has done so. He/she would be required, by professional practice, to communicate the potential concern to the nursing supervisor as well. Communication is vital in healthcare. We all know this. Also, if one doesn't document something, by law, it wasn't considered done. Knowing, however, that communication is vital for safe practice, he/she must follow-up on the given information in a timely manner and document that carefully as well. You'd think to at least cover her/his own butt, he/she would have included the date, time, and fact that she made the covering physician aware, what the doc's orders were and the effects of the interventions, if there were any ordered. You keep it simple, but it still has to be documented.
Everyone needs to function to the level of their SOP, always keeping best practices in mind. Supposedly the nurse was given this relevant information from the patient. If the nurse documented this fine, but the nurse is responsible to go beyond that. None of us practices in a vacuum. Part of his/her plan of action, interventions, and evaluation of those depends on her/him communicating such relevant and information to the physician in charge. It is b/c he or she can and should be held to maintaining the SOP by law under his/her licensure that he or she should then also document responses of the communicated information and medical plan from the physician.
It's a team mission caring for sick people and helping to maintain or optimize wellness for people. It's not about who is the ultimate boss. I can dig and do respect the physician in charge, and I have no problems communicating with her or him. I also have no problems documenting, b/c it's absolutely essential. It's about working together for the sake of the patients and others. At the very least, the nurse had an ethical, public-health responsibility to report this and document adequately. Personally, if I were the nurse manager and/or director over this nurse, he/she would be pulled in for administrative action. The nurse fell short of not only good sense, but what the law considers as her responsibility under her/his license. I'd be surprised if the nurse doesn't get some kind of disciplinary action if it proves true that she didn't report the information to the physician, document that information, and follow-up appropriately with it.
As for the physician, I'm not one yet; therefore, I will just report what the news shared, and that I personally feel that if people are educated to take relevant histories--and in light of the abundant news, they would pay special attention and ask relevant questions--following CDC guidelines. I wasn't there and I don't know what was going on with the physician. But I do think that the nurse had an obligation to report this information to the physician, if indeed he or she did not. If so, why the nurse didn't report and follow-up is beyond me. It's not like this Ebola business hasn't been media-blasted everywhere. But yea. Unless one was there or has all the pertinent information, it's unfair to state absolute judgments. In practice, we get stressed or become too comfortable. This scare should get people's attention though and make them think twice.
I also agree that this patient probably knew when he left Liberia that he was putting others at risk, but he probably was scared and wanted to hightail it out of there to the US ASAP. I mean, who wouldn't want to go where they would get the best care and the best treatments for survival? I think that is why he communicated this to the ED nurse after omitting that information before leaving Africa--that is, if all the information given proves true. He probably didn't expect the nurse or anyone else to drop the ball.
great point. there's tons of studies and whole careers based on improving this issue. in a busy ER it's difficult for the triage RN to literally find and tell a doc. usually triage will call the charge RN then from there the information is disseminated. there's no rule of thumb except for judgement. if something is scaring the charge RN, they'll usually find a doc and rightfully so. if a seasoned nurse is worried about something sitting in triage, i need to know. I am still having trouble believing this triage scenario. it's one thing just to write on the chart in triage, "lethargic"and drop the ball but a guy walks in and says "ebola" to the nurse. that gossip will spread faster than which nurse is banging dr X this week.Beyond all of that, hell, don't doctors and nurses actually talk to each other anymore? This is one of those kind of things where the nurses and doctors need to have "hand and mouth disease"--typing in the information or writing it by hand AND opening their mouths to communicate. Does this ED not work with open communication between nurses and doctors? I am perplexed.
Honestly, this forum truly amazes and baffles me at times. Do you actually think this?
Do you even have a test you can order to confirm Ebola, before you dispo a patient?
The best you could ever do in the ED is to diagnose "Viral Syndrome, rule out Ebola." There's nothing "100%" about that. In fact, you're more likely to admit 100 of those and at best, have 1 turn out to be Ebola, cripple your hospital by filling all their beds with viral syndromes and lead everyone to think that you think every flu is Ebola. That puts your diagnostic accuracy much closer to 1%, not 100%. More likely it will be closer to 0%, since you still might not ever see Ebola.
Do you think Ebola is new?
Ebola is not new. It's been around for decades. So has Hantavirus. Are you going to be 100% accurate on diagnosing that, too, if you ever see it? That's a disease as bad a Ebola, and actually has occurred hundreds of times in the US, compared to the 1 case of Ebola diagnosed in the US, to date.
What about MERS virus? Do you have a one hundred percent chance of seeing a patient in the ED and putting a diagnosis of "MERS" on their chart before they leave your ED?
Eastern Equine Encephalitis: You got that one too.
Malaria? You're probably 100% on that one, too, because you can focus in like a laser beam by asking about viral symptoms and travel. Yet you "rarely" even ask about travel:
Hmm...
You just rely on your triage nurse to make the diagnosis of this disease with a mortality rate that averages 50%:
Hmm..
So, you're 100% accurate in diagnosing Ebola, when you have no diagnostic test, no CT scan, X-ray or ultrasound that will show it, and when the only diagnostic "tests" in your tool bag is to ask two questions about, 1- non-specific viral symptoms and, 2- travel history, neither of which by themselves can make any specific diagnosis whatsoever?
You're 100% accurate, even when a case could present exposed by secondary contact, with no travel history whatsoever and no knowledge he was ever exposed?
When you ask him your screening questions he answers, "No" because he really doesn't think he's sick, doesn't want to get isolated for weeks or create a panic?
Or because he happened to shake the hand of a guy, who shook the hand of a guy who never traveled to Africa in his life, but who used a toilet in an airport somewhere in Europe vomited on by a guy who got sick after getting off a connecting flight from Liberia, and has no clue he was actually exposed to Ebola?
Wow. Truly amazing, in many more ways than one.
but this is not some podunk ED staffed by some non-BC FP.
The patient was admitted to Community Hospital in Munster, Indiana, on April 28, the same day he visited the emergency department there, the health department said. He has been isolated and is in stable condition.
Will state again: I would 100% not miss this diagnosis. It's not because I'm some master practitioner. Its because the CDC mandates every human being who comes into the ER stable is asked IN TRIAGE if they have been to Africa in the last 28 days, and then to get a temperature if they say yes. This isn't falling in your shoulders, it's the administration and nursing because that's where the screen is protocalled (and in many states mandated) to occur.
Its a mistake to not ask viral syndrome patients a travel history, but I rarely ask in honestly. But since I'm not the one screening them, I'm assuming they came pre screened.
1) CDC says every human being who enters the ER should be asked if they traveled to Liberia, Siera Leone, Nigeria or that fourth country that is on the (literally) twenty five maps posted between all the ER entrances and the end of both walk in and EMS triage.
2) this screen is done at triage and the patient cannot be put into a the ER unless they are critical or an answer of "no" can be confirmed. Critical patients are revived and bloods are identified as BIOHAZARD bloods for your lab until they can be asked about travel history or they expire.
3) if they say yes they are asked if their complaint includes fever, body aches, nausea, or cough. Also a temp is taken immediately.
4) a yes in section 3 leads to them immediately going to an isoolation room and a call being placed to the CDC.
5) the CDC then runs the patient for you and takes responsbility for directing the exam to rule Ebola out.
If you can follow five steps above, the only way you're missing Ebola is by your hospital choosing to not follow the criteria, the patient lying about his travel history at triage, or the patient dying during the initial resuscitation. I could be a third year med student and get 100% accuracy for any patient that isn't lying as long as I know how to listen to the CDC on the phone and how to perform the bare basic history and physical the guy on the phone asks for. The physician DOES NOT make any clinical decisions until the CDC has ruled out Ebola for you with this screening method.
Couldn't agree more with this post! Where's the solidarity people? Before med school I spent a good amount of time in the presence of cops and firefighters. You know what they do really, really well? They watch out for each other. They get each others backs. They work in very dangerous environments and over time have learned that united they stand and divided they fall. If a news story breaks that reports some purported wrong doing by a cop, and it's not some egregious crime against humanity, every cop I know will automatically defend the accused cop. What happens if you hit a cop? Five of his cop buddies take you out back and beat the crap out of you.
Physicians are the complete opposite of this. Constant in-fighting seems built into the House. ED doc missed the zebra, ortho can't manage HTN, blah blah blah. So much bickering. And think about what happens if you punch a physician? Do his buddies take you out back and kick your butt? Nope. Absolutely nothing happens. Not saying we should start beating up anyone who punches a doc but we do need to learn to stick together. We need to change our culture such that we are all watching out for each other. If we actually fought like a team maybe WE, not the lawyers and politicians, could shape our health care system the way it should be shaped.
Here's the problem I think people have with what you're saying: You would 100% not miss this diagnosis, but in making that bold claim, you're actually not doing anything to make the diagnosis based on what you're telling us. So you're taking all the credit for a system that's in place where you are, and blaming the physician at a place where this same system is apparently not in place.
So you're relying on the nurses to ask this. Kind of like the physician in Texas. Someone slipped through the cracks, either because it wasn't documented properly or because he didn't see that it was documented. Sounds exactly like what you're doing, and if your system breaks down, you're going to almost always miss it, just like this guy did.
Again, what's your role in this? Is it "nothing," or "assessing the patient for other medical conditions and trusting other people have done the work to rule out Ebola?" Whichever you prefer. I'd personally opt for the latter, since it seems a little more flattering, but they're essentially the same thing. What if the nurse asks and they admit to travel, but she's on autopilot and hits the box for "no travel" while hammer-clicking through all the other crap the EMR presents her with? Or they just fail to act properly to positives in #2 or #3 and don't place the patient in isolation or call the CDC? How do you stop these errors from others from impacting your perfect record?
I rarely, if ever, ask about travel history in someone with a fever. Hopefully this thread will prompt me to do so from here on out, as I'm in locations where people are unlikely to be travelling internationally as Veers said. I very well may have missed this patient too, and it sounds like you're in the same boat. I'll own that. But you're claiming you would "100% not miss this diagnosis," despite doing nothing to prevent missing it. You don't see the disconnect here?

Actually the cost is pretty substantial. We have one hospital in our whole system that is set up to deal with Ebola, which they created by carving out a chunk of ICU beds that could be used for other purposes. Ambulance transport and decon are also quite expensive. Then there's the issue of patient's with critical disease that isn't Ebola. I don't know if you have cared for one of the + screen patients, but there's about a 6-8 hr period where you can't really exam them. And I'm not sure if you're using "very rare false positive screen" to refer to the total number of febrile visitors from Africa or to refer to very few of those patients not having Ebola. Because as I'm sure you're aware the specificity is poor (most patients meeting case definition will have another virus or malaria) for the screening criteria.
Given the number of patient contacts and the fact that most processes have multiple failure modes, your "perfect storm" of slip-up is actually going to be somewhat common. I understand it's super easy to blame people for protocol violations (the "fire the nurse the next day" approach), but it's actually pretty difficult to operationalize a lot of the CDC/JC/Medicare recommendations. Especially with care focused significantly more on tasks than patients, lack of a proper EMR prompt will almost guarantee the system will fail at some point.
I agree. Just like there is no test, imaging study, prediction rule or diagnostician that is 100% sensitive, neither is any "triage screening algorithm" that is 100% sensitive, CDC generated or not. So to criticize a specific doctor about such a thing in public without knowing specific details first hand, is naive at best, foolish and arrogant worst, and just shows a complete misunderstanding of the entire concept of testing and diagnosis, and how such processes always have inherent imperfections at every step along the way, including those within each and every one of us.Because as I'm sure you're aware the specificity is poor (most patients meeting case definition will have another virus or malaria) for the screening criteria.
Given the number of patient contacts and the fact that most processes have multiple failure modes, your "perfect storm" of slip-up is actually going to be somewhat common.
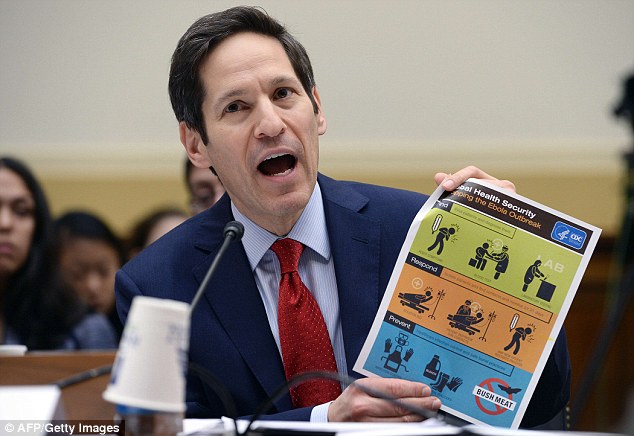
I have not seen a single one of these signs (still) in the multiple EDs I work at in Texas. Are you talking about this thing? http://i.dailymail.co.uk/i/pix/2014/08/08/1407497116091_wps_1_US_Centers_for_Disease_Co.jpg1) CDC says every human being who enters the ER should be asked if they traveled to Liberia, Siera Leone, Nigeria or that fourth country that is on the (literally) twenty five maps posted between all the ER entrances and the end of both walk in and EMS triage.
I've looked up and down the CDC website and still have no idea what you're talking about.The issue here is this Texas hospital chose not to follow the CDC guidelines. the NYSDoH took that choice away from NY hospitals. Don't follow the guideline and this is infinitely more difficult to assess. Follow the guideline and you find out Ebola is like HIV: there is no way you are exposed to Ebola and don't have a damn good idea that you might have been, so it's easy to rule out on history if your asking the right questions; which the CDC asks for you.
I have not seen a single one of these signs (still) in the multiple EDs I work at in Texas. Are you talking about this thing? http://i.dailymail.co.uk/i/pix/2014/08/08/1407497116091_wps_1_US_Centers_for_Disease_Co.jpg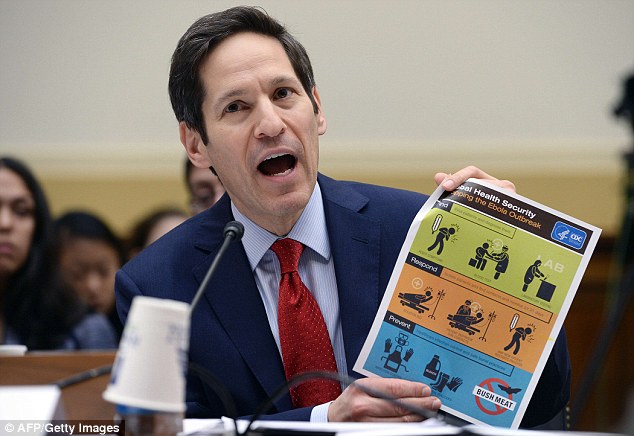
I've looked up and down the CDC website and still have no idea what you're talking about.
Just was looking at the latest CDC interim guidelines and unless they lied about his temp to the press, the patient would not have met criteria for being Person Under Investigation (PUI) on his initial eval. So swing and a miss on your 100% sensitive idea.Nope it's a decision nonogram. We have two nearly identical ones, one with the CDC logo and one with the NYSDoH logo on it.
Just was looking at the latest CDC interim guidelines and unless they lied about his temp to the press, the patient would not have met criteria for being Person Under Investigation (PUI) on his initial eval. So swing and a miss on your 100% sensitive idea.
the Spanish govt killed her dog too, apparently they can carry it?And a nurse's aid in Spain was diagnosed, likely from having the glove hit her face when she was removing it. I'm just praying that the Dallas patient didn't infect anyone here.
and now it only gets worse. what's next?Well, that guy from Dallas died from his ebola today.
They also don't have doctors with 100% diagnostic accuracy, like our very own DocEspana.
You may be right. But personally, I thought it was a little bit "unnecessary" to publicly criticize a fellow physician, who certainly cannot publicly defend him-/herself due to HIPAA and medical-legal reasons, in a case where the person criticizing had no first hand knowledge, but used the unfair advantage of retroscopic vision, on the grounds that he has 100% diagnostic accuracy in relation to a disease he's seen zero cases of. I want better than that for myself, for you, and for him, too.C'mon, man...that wasn't necessary. I mean, I think the guy likes to hear himself talk, and perceives himself to be a polymath scholar, but just let it go.
I work in a community hospital in North Carolina. One of our docs is pretty anxious about our preparedness, which is fair since our mothership recently sent us a plastic bin with a piece of paper taped to the top that says "Ebola response kit" and contains a plastic gown, a facemask, and a pair of booties in it...yikes.
It sounds like some of you folks are working in MUCH better prepared places, probably because you have major international airports nearby.
Given that the above discussion may have devolved a bit...It would be helpful for me and I suspect others to hear some of the basic plans you have in place as I've been debating what to do if a potential Ebola patient lands in my ED. The questions below are very basic but alarmingly our ED group has not been given clear instructions on different conceivable scenarios.
1. If screening is successful and a nurse picks up on a potential Ebola patient in a triage room: what then? Do they stay in the triage room for hours until appropriate authorities are contacted? Get moved back to isolated area in ED?
2. Let's say they are in the ED somehow: do they get 1:1 coverage by a physician and a nurse? I would assume so. Do you then call in extra physician back-up to keep the dept running? I find it a bit alarming that the Spanish nurse contracted Ebola. This was an advanced hospital with serious protective gear and she got it because 'maybe' her gown touched her face? Doesn't sound so difficult to contract to me.
3. How do the other patients in the ED respond to docs and nurses being spotted in 'space suits' if that's what is used? How do you prevent panic?
4. What if your Ebola patient comes via EMS and is promptly isolated...and his family shows up in the WR 10 minutes later touching counters/chairs, etc: what then? Quarantine them and check temps and hope no fevers?
While the possibility of Ebola coming to my ED is low I worry about how quickly things could go wrong.
once i saw him on the news, that's exactly the problem that I'd knew would surface. let's face it, jesse wasn't there b/c ebola hit the states. he's there cause there's a pot to stir. dallas pres has been under so much pressure I am sure they bent over backwards for the patient and family. yes it's unfortunate the guy died but he did contract an extremely deadly virus that we have no cure for. granted he did want any desperate human would do by lying and hopping over here to get 1st class care but exceptional care doesn't mean a cure.Also, I can't handle all of this nonsense with Jesse Jackson, and the family claiming that the patient got subpar care because he was black. "Why did all of the white people live and the black man died" Ugh its disgusting. What doctor would ever give someone subpar care based on their race? not even the worst doctor would do that. Not to mention- this hospital is already suffering a PR disaster due to the miss on the ER's part- seeing as they're in the spotlight I would think they did everything in this power to help this man survive.
I've been wondering the same. I saw the ideal "drill" on abc showing ems gowning/masking the suspected ebola pt, transferring the pt outside in the ems bay, then nurses already gowned with the stretcher entering through the decon room and placed in an isolation room. sounds great, the pt is pre wrapped like a burrito before entering the building. chance of spreading anything is pretty much down to 0. what about the guy that walks into triage, coughing, vomiting, spitting up blood....etc. won't the triage room and RN be contaminated?The problem is what do you do with a positive screen who is unstable (even though much more likely they have sepsis or malaria or another issue causing them to be ill rather than actual ebola)?
Lawsuit time!
Who will have a hard time, the plaintiff?Every tv expert is saying they'll have a hard time finding a lawyer in TX.. or a sympathetic judge or jury. maybe the hospital will settle to avoid further harassment by Jesse Jackson
Who will have a hard time, the plaintiff?
Mr. Duncan infected a nurse. The question is how many more??
F@$@. "The protocol works but even a single lapse can result in infection. " - from CNN article. I would suggest that it doesn't work since we've had two first world infections among healthcare workers. But so easy to blame protocol violations rather than admit it can't be followed or it's not as effective as it should be.
How are you going to protect yourself? Is wearing isolation gear enough? What about your stretchers, the ambulances, your helicopters? What do you do with them once you put a patient in one after you slapped a "rule out Ebola" on their chart?
Can the chopper still fly, doc? Can the ambulance still run, doc?
You think you are ready, but are you? The nurse in Texas thought he/she was ready, and per news reports, wore protective gear.
Was the protocol broken?
Or is the protocol ineffective even when followed?
It's here.
