- Joined
- Sep 25, 2012
- Messages
- 1,624
- Reaction score
- 2,365
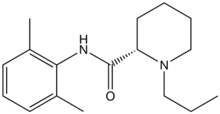
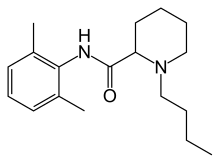
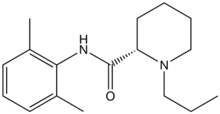
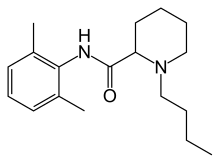
So I got pimped by one of my fav attendings the other day. He told me that one could add epinephrine to a bupivacaine block but not to a ropivacaine block because ropivacaine is a vasoconstrictor. I've heard this notion before, but it always struck me as odd, how would a local anesthestic that blocks sodium channels be a vaso constrictor???!?! specially since bupivacaine has such a similar structure and obviously vasodilates?? (TL;DR at bottom)
Ropivacaine:
Bupivacaine:
Original Kopaz article that showed lower blood flow with ropiv compared to bupiv:
Kopacz DJ, Carpenter RL, Mackey DC. Effect of ropivacaine on cutaneous capillary blood flow in pigs. Anesthesiology. 1989;71:69–74.
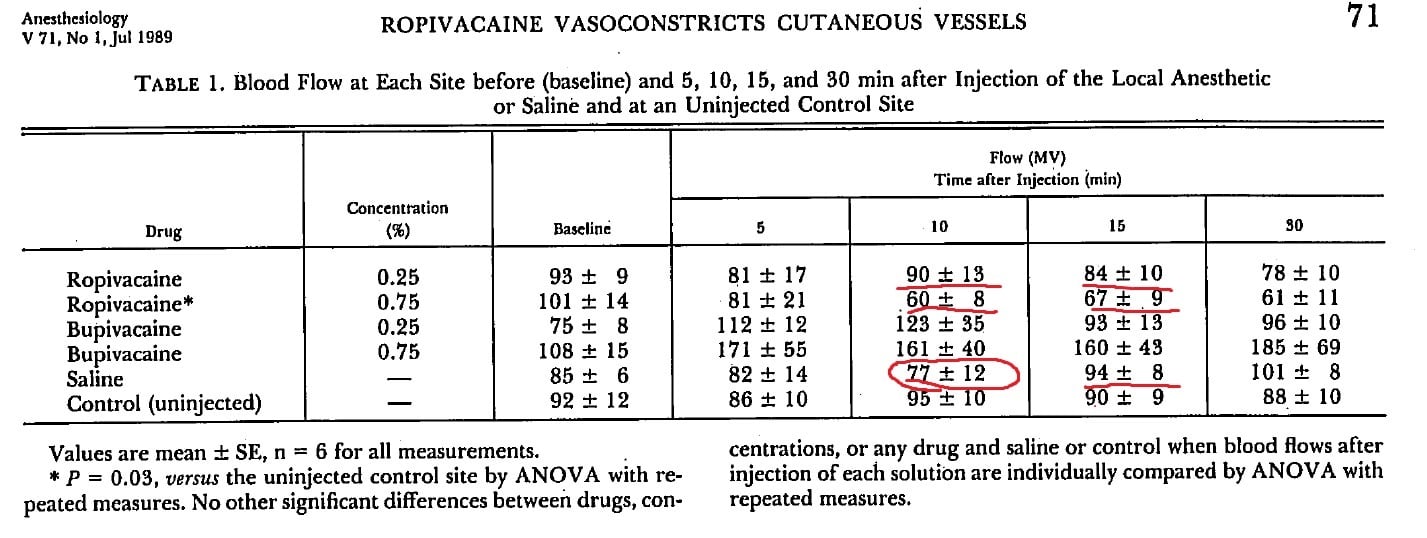
I'm not sure if this data is enough to make me believe that ropivacaine is a vasoconstrictor. But cocaine, another local anesthetic, is definitely a vaso constrictor.
Cocaine:
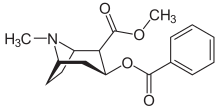
But the vasoconstriction is probably due to the side chain.
3 years after kopaz, this guy in sweden named Cederholm actually did the same study but he added epi to ropiv:
Cederholm I, Evers H, Löfström JB. Skin blood flow after intradermal injection of ropivacaine in various concentrations with and without epinephrine evaluated by laser Doppler flowmetry. Reg Anesth. 1992;17:322–8.
But his study actually showed that Epi + ropiv lowers blood flow compared to ropiv alone.
So in my mind this at least proves that epi + ropiv vaso constricts more than ropiv alone. But does it really matter clinically?
Hickey R, Blanchard J, Hoffman J, Sjovall J, Ramamurthy S. Plasma concentrations of ropivacaine given with or without epinephrine for brachial plexus block. Can J Anaesth. 1990 Nov;37(8):878-82
This article shows that the plasma concentration of ropiv is no different during subclavian blocks whether or not if you have epi added. but the study is small and the data is all over the place, not convincing to me.
Schoenmakers KP, Fenten MG, Louwerens JW, Scheffer GJ, Stienstra R. The effects of adding epinephrine to ropivacaine for popliteal nerve block on the duration of postoperative analgesia: a randomized controlled trial. BMC Anesthesiol. 2015 Jul 10;15:100. doi: 10.1186/s12871-015-0083-z.
This article shows that mean time to asking for first opioid, which is clinically what really matters, does not chang with epi vs no epi in ropiv blocks.
TL;DR:
- Evidence for ropiv as a vaso constrictor is weak, it just doesn't vasodilate as much as bupiv.
- However, clinically, it doesn't seem to affect the duration of blocks clinically if you add epi to ropiv.
Finally, epi as marker for intra vascular injection marker has its own merits. However, with good ultrasound technique, it feels like that might be marginal at best.
Thoughts? all discussions welcome. What do you do in your practice, why? Does any of the above info persuade you to think about changing your practice?
Ropivacaine:
Bupivacaine:
Original Kopaz article that showed lower blood flow with ropiv compared to bupiv:
Kopacz DJ, Carpenter RL, Mackey DC. Effect of ropivacaine on cutaneous capillary blood flow in pigs. Anesthesiology. 1989;71:69–74.
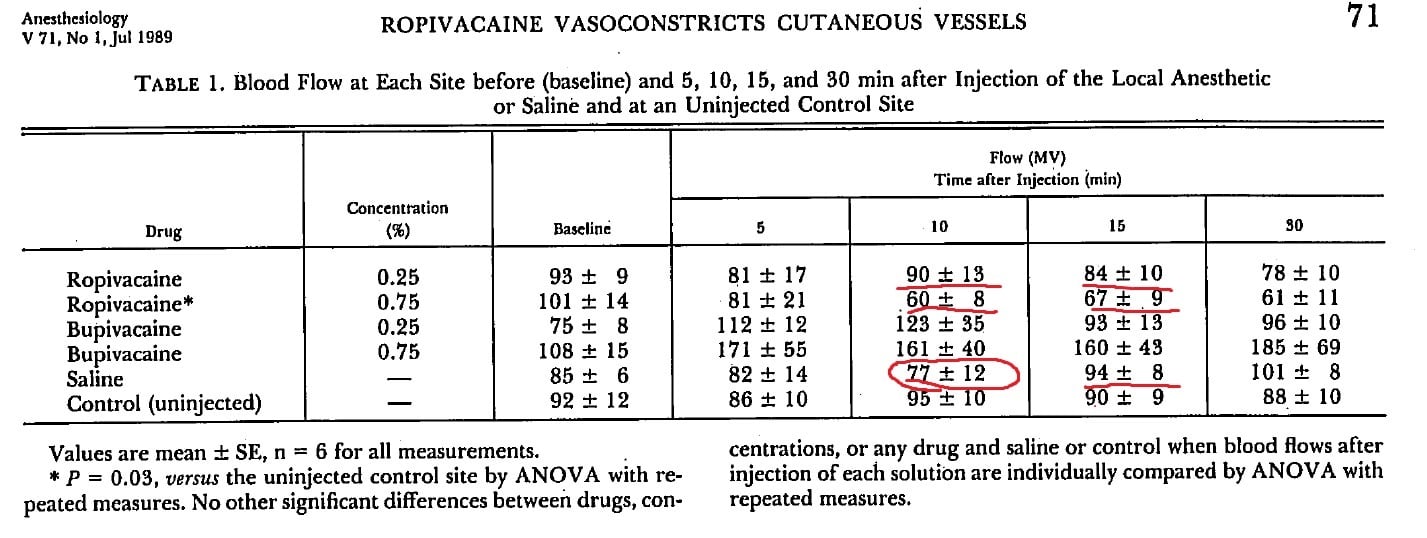
I'm not sure if this data is enough to make me believe that ropivacaine is a vasoconstrictor. But cocaine, another local anesthetic, is definitely a vaso constrictor.
Cocaine:
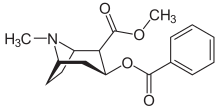
But the vasoconstriction is probably due to the side chain.
3 years after kopaz, this guy in sweden named Cederholm actually did the same study but he added epi to ropiv:
Cederholm I, Evers H, Löfström JB. Skin blood flow after intradermal injection of ropivacaine in various concentrations with and without epinephrine evaluated by laser Doppler flowmetry. Reg Anesth. 1992;17:322–8.
But his study actually showed that Epi + ropiv lowers blood flow compared to ropiv alone.
So in my mind this at least proves that epi + ropiv vaso constricts more than ropiv alone. But does it really matter clinically?
Hickey R, Blanchard J, Hoffman J, Sjovall J, Ramamurthy S. Plasma concentrations of ropivacaine given with or without epinephrine for brachial plexus block. Can J Anaesth. 1990 Nov;37(8):878-82
This article shows that the plasma concentration of ropiv is no different during subclavian blocks whether or not if you have epi added. but the study is small and the data is all over the place, not convincing to me.
Schoenmakers KP, Fenten MG, Louwerens JW, Scheffer GJ, Stienstra R. The effects of adding epinephrine to ropivacaine for popliteal nerve block on the duration of postoperative analgesia: a randomized controlled trial. BMC Anesthesiol. 2015 Jul 10;15:100. doi: 10.1186/s12871-015-0083-z.
This article shows that mean time to asking for first opioid, which is clinically what really matters, does not chang with epi vs no epi in ropiv blocks.
TL;DR:
- Evidence for ropiv as a vaso constrictor is weak, it just doesn't vasodilate as much as bupiv.
- However, clinically, it doesn't seem to affect the duration of blocks clinically if you add epi to ropiv.
Finally, epi as marker for intra vascular injection marker has its own merits. However, with good ultrasound technique, it feels like that might be marginal at best.
Thoughts? all discussions welcome. What do you do in your practice, why? Does any of the above info persuade you to think about changing your practice?
Last edited: