Hospitalist salaries have definitely gone up in the past decade. According to this report (
Key trends in hospitalist compensation from the 2020 SoHM Report) it went from median of $215k in 2010 to $307k in 2020. Even after adjusted for inflation, that's about a 21% increase in pay over a 10 year period. If this trend continued you would expect the median hospitalist compensation to be around $370k in 2030 (in 2020 dollars).
Not sure if that trend will continue for the next decade though. There are a few things going against further large increases in hospitalist compensation, including tendencies for reimbursement cuts from Medicare every year, potential to use more midlevels as extenders (without technically replacing attendings), and the fact that the job market is already getting saturated in the big cities, and that hospitalist medicine has a relatively low entry barrier compared to other specialties. Any IM or FM grad can do it and these are the 2 largest and least competitive specialties to match into. It's become popular that even a good amount of FM grads are getting into it (and traditionally FM residency has emphasized more outpatient medicine while IM residency tends to be more inpatient focused), and even some fellowship trained sub-specialisits like Nephro and ID are doing it since in the the recent market it has paid more per hour than the lower paying IM subspecialities.
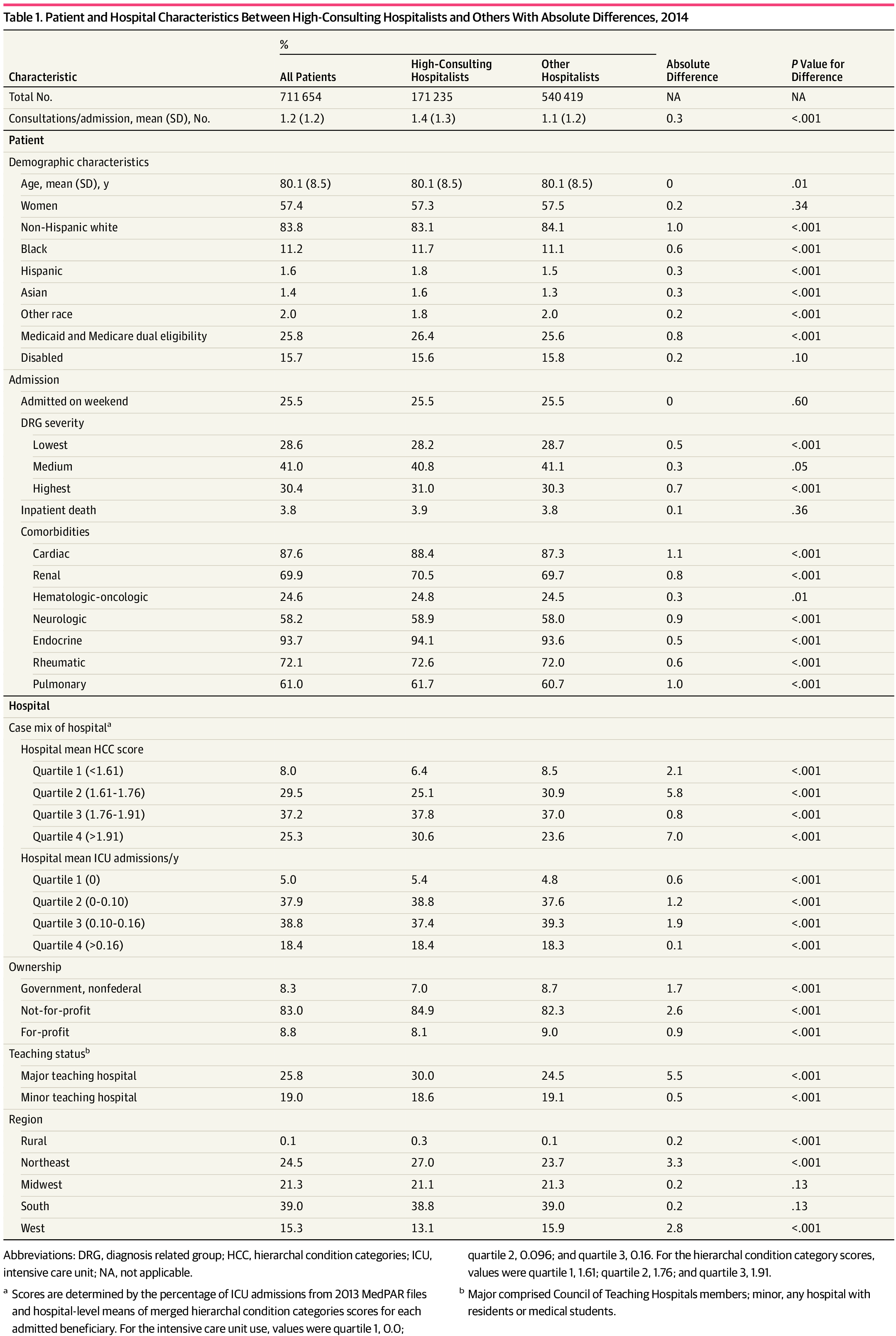
Minimizing consults doesn't really save the hospital money. Consults are additional E/M that the other specialties can bill for, and many places they want the business (especially if there's 2 or more groups in the same specialty competing for business at the same hospital).