Attending GI. Its interesting how both the food impaction and UGI bleeding threads have taken off.
Unlike a food impaction where I agree that I would always like a secured airway, it is not nearly as straightforward in the setting of upper GI bleeding. In fact, this has been recently looked at and there were MORE complications in the group that was prophylactically intubated. These were ivory tower Cleveland Clinic patients:
Association of prophylactic endotracheal intubation in critically ill patients with upper GI bleeding and cardiopulmonary unplanned events. - PubMed - NCBI
"
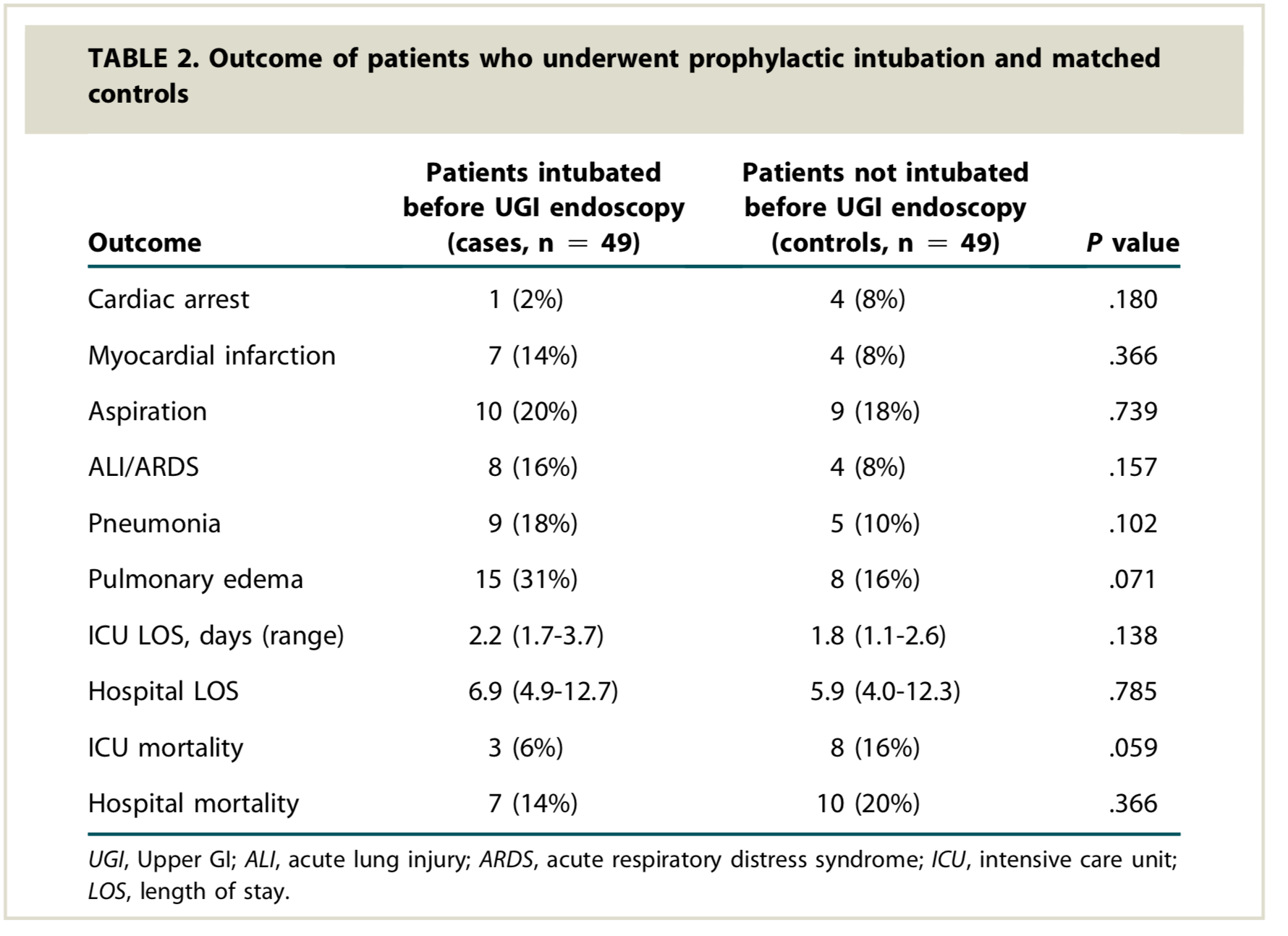
RESULTS:
Two hundred patients were included in the final analysis. The baseline characteristics, comorbidity scores, and prognostic scores were similar between the 2 groups. The overall cardiopulmonary unplanned event rates were significantly higher in the intubated group compared with the nonintubated group (20% vs 6%, P = .008), which remained significant (P = .012) after adjusting for the presence of esophageal varices."
This is a high quality journal from a high quality author.
We need to think more critically about these situations other than tube = good.
There is a problem that you and your GI friends are missing: these are not aspiration-related outcomes. These are cardiopulmonary complications that come either from inducing the critical patient for intubation, from positive-pressure ventilation, or from poor post-intubation ICU care (e.g. sedating a hemodynamically-sensitive patient with propofol).
What this single-center retrospective study (I assume because I can't read it) has proven is that,
at Cleveland Clinic, the ICU care sucks enough that it's better to not intubate a bleeding critical patient for an EGD.
FYI, I am an anesthesiologist-intensivist. As an intensivist, I only intubate when I have no choice, always thinking about what that will do to my patient's physiology (e.g. it can crash a bad RV). As an anesthesiologist, I do it when I am concerned about a significant risk of aspiration. Do you know how much you need for aspiration pneumonia? About 0.2 ml/kg of body weight. That's 15 cc for the average adult, not much. And, let me tell you, aspiration pneumonia in a critical patient can be a killer, the tombstone, exactly because there is no reserve.
Few gastroenterologists realize that an EGD can be almost as stimulating as a videolaryngoscope intubation. I can do either with just midazolam (and some fast/short-acting muscle relaxant for the latter), with a semi-awake patient who won't remember crap, despite having an EF of 10%. That's the magic of anesthesia
and anesthesiologists.
What I cannot do, as an anesthesiologist, is teach proper ICU care to the arsehole ICU attendings who are not around to take care of their critical patients and prevent post-intubation problems (if the patient cannot be extubated at the end of the procedure). That's not something to leave to trainees or nurses. I also cannot eliminate intubation-related crashes because of stupid (mostly unsupervised) anesthesia trainees who, for example, push a ****ton of medication for intubation (yes, people can crash even with etomidate), which is another problem one would clearly notice in a big academic place such as Cleveland Clinic, and much less likely to happen in a community hospital.
And before one starts spewing around "evidence-based medicine", one should be so kind to learn to actually interpret the value of the "evidence", and learn to separate the truly good science from the resume-padding pseudoscience (hint: most of the retrospective studies). Otherwise, one will harm more patients than help. What some gastroenterologists call "evidence" is downright laughable: I remember being an intern and a GI protocol in widespread use in the US was based on a joke of a Chinese study.
ONE CANNOT EXTRAPOLATE A SINGLE-CENTER RETROSPECTIVE STUDY DONE IN AN ACADEMIC PLACE TO MOST HOSPITALS IN AMERICA, BECAUSE THEN ONE IS LIKE THE IDIOTS WHO SAY THAT MEDICAL ERRORS KILL 100,000 PATIENTS EVERY YEAR. Before drawing conclusions from a sample, one has to prove that the sample is truly representative for the large population.
P.S. My best friend is a gastroenterologist. And, as I said, I am also an intensivist, which makes me approach every study with a healthy dose of skepticism. (Just look up the Surviving Sepsis
Crap Campaign controversy.)