After starting intern year back in July, I've been finding that I don't really love residency. I think it is interesting (most of the time), gets me where I want to go fellowship-wise, and is better than my alternatives... but I'm certainly not loving it. I'm surprised, because even when I was working a lot as a med student (and had to work >80h weeks) I was enjoying it more than I am now. How are the rest of you feeling about residency? Is it just being an intern or do/did most of you enjoy it the entire time?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
How much do you/did you like residency?
- Thread starter DNM
- Start date
- Joined
- Mar 6, 2005
- Messages
- 21,376
- Reaction score
- 17,903
It's that. And it's going to get even more fun come February.After starting intern year back in July, I've been finding that I don't really love residency. I think it is interesting (most of the time), gets me where I want to go fellowship-wise, and is better than my alternatives... but I'm certainly not loving it. I'm surprised, because even when I was working a lot as a med student (and had to work >80h weeks) I was enjoying it more than I am now. How are the rest of you feeling about residency? Is it just being an intern or do/did most of you enjoy it the entire time?
D
deleted547339
After starting intern year back in July, I've been finding that I don't really love residency. I think it is interesting (most of the time), gets me where I want to go fellowship-wise, and is better than my alternatives... but I'm certainly not loving it. I'm surprised, because even when I was working a lot as a med student (and had to work >80h weeks) I was enjoying it more than I am now. How are the rest of you feeling about residency? Is it just being an intern or do/did most of you enjoy it the entire time?
You probably feel incompetent and are having to do a lot of scutwork. Internship sucks. You're normal.
- Joined
- Dec 14, 2006
- Messages
- 69,368
- Reaction score
- 61,670
After starting intern year back in July, I've been finding that I don't really love residency. I think it is interesting (most of the time), gets me where I want to go fellowship-wise, and is better than my alternatives... but I'm certainly not loving it. I'm surprised, because even when I was working a lot as a med student (and had to work >80h weeks) I was enjoying it more than I am now. How are the rest of you feeling about residency? Is it just being an intern or do/did most of you enjoy it the entire time?
I didn't "love" parts of residency but still look back on it as one of the best times in my life. Mostly the people I guess. I imagine it's like people who go through combat together. You don't miss hiding behind a wall when you are being shot at, but the people, the camaraderie, the shared experience . . . they mean something. It's a bit ineffable.
The lack of ultimate responsibility was also nice. Something you simply can't appreciate until you are out on your own. You only see how cool that was in retrospect. No way to appreciate that kind of thing *IN* training.
- Joined
- Dec 14, 2006
- Messages
- 69,368
- Reaction score
- 61,670
It's that. And it's going to get even more fun come February.
I wish someone would have told me it's darkest right before the dawn . . .
You gotta hold on until March. The spring. The longer days. The warmer temps. It. Gets. Better.
- Joined
- Jan 2, 2014
- Messages
- 11,384
- Reaction score
- 24,014
Medicine intern year sucks
All the mean consults
The ****ty surgeons
Writing all the notes and doing all the scutwork
Getting blamed for things that aren't your fault
The only good thing was the people. If your senior sucked, you were in for a bad time.
All the mean consults
The ****ty surgeons
Writing all the notes and doing all the scutwork
Getting blamed for things that aren't your fault
The only good thing was the people. If your senior sucked, you were in for a bad time.
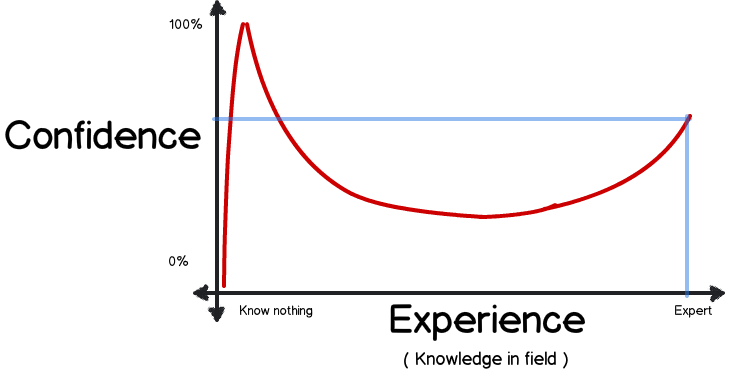
Began my internship on July this year and I feel quite the opposite. A bit euphoric in fact. I like it very much and I don't feel useless most of the time at least on the floors. Doing electives I do feel kind of clueless am not familiar with some of the small details of more complicated patients. I still kind of feel like a medical student while on elective (AKA cardiology/pulm/etc). But in the floors I feel reasonably comfortable. Obviously there is a lot I have still to learn, both in terms of medical knowledge and in terms of how the hospital work but even right from the start I don't feel completely useless. I have lost the "hesitation" to order some labs/tests on my own without consultation with seniors/attending and even some meds. I still discuss everything I do for the sake of communication and/or if I inadvertently did the wrong thing (which I have) but so far it going well and I enjoy it.
Hours are hard, but not crazy so far most days are less than 12h with a few 8h sprinkled over. I don't have 2 days weekends unless electives or clinics every 4 weeks but that is not bad either.
Could it be better? Ofcourse but I feel very comfortable at the moment.
What in particular are you having trouble with?
Hours are hard, but not crazy so far most days are less than 12h with a few 8h sprinkled over. I don't have 2 days weekends unless electives or clinics every 4 weeks but that is not bad either.
Could it be better? Ofcourse but I feel very comfortable at the moment.
What in particular are you having trouble with?
D
deleted547339
Began my internship on July this year and I feel quite the opposite. A bit euphoric in fact. I like it very much and I don't feel useless most of the time at least on the floors. Doing electives I do feel kind of clueless am not familiar with some of the small details of more complicated patients. I still kind of feel like a medical student while on elective (AKA cardiology/pulm/etc). But in the floors I feel reasonably comfortable. Obviously there is a lot I have still to learn, both in terms of medical knowledge and in terms of how the hospital work but even right from the start I don't feel completely useless. I have lost the "hesitation" to order some labs/tests on my own without consultation with seniors/attending and even some meds. I still discuss everything I do for the sake of communication and/or if I inadvertently did the wrong thing (which I have) but so far it going well and I enjoy it.
Hours are hard, but not crazy so far most days are less than 12h with a few 8h sprinkled over. I don't have 2 days weekends unless electives or clinics every 4 weeks but that is not bad either.
Could it be better? Ofcourse but I feel very comfortable at the moment.
What in particular are you having trouble with?
Take a pause. You're going to be the second year resident that kills people. I'm not saying this to be mean, but as an intern in the fall you know very very little. You should still be very, very afraid.
So you recommend to instead be a frighten useless doctor instead? There is a is a fine line between being confident and careful and frighten and useless and I agree this line is kind of blurry, hard to see and I even doubt any doctor ever knows the difference. We all made mistakes and at one point or another we will all do some degree of harm. Most of the time knowingly (as part of a side effect) but sometimes also by mistake or even negligence. Fear, however is not the proper response.Take a pause. You're going to be the second year resident that kills people. I'm not saying this to be mean, but as an intern in the fall you know very very little. You should still be very, very afraid.
Yes, I am only a 1st year intern but I am also and MD and I have to take responsibility and initiative otherwise the last 4 years were simply a waste of time.
I am not going to kill anyone for ordering a bunch of blood tests, X-rays, ultrasounds or EKG on my own. I am not going to kill anyone by ordering some cough medicine, Tylenol or some nebulizer inhalers. I am not going to kill someone by giving some fluids to someone that is not on CHF and that does not have some electrolyte imbalance such as hypo/hypernatremia, I am not going to kill someone for putting them NPO just because I am suspecting a weird diagnosis that might require a procedure.
Ofcourse I am careful with those medications that have more serious side effects. I am not going to be ordering heparin haphazardly without discussing it with the attending previously. But the only way to learn properly is to lose the training wheels and I think being comfortable with some simple decisions is definitely the first step. I have always discussed every single med I have given to my patients with attending and/or senior resident and asked feedback and if I did the correct thing. I do not necessarily discuss blood tests or imaging such as x-ray or ekg unless it comes back negative and I was not sure if I needed such test. So far I have got very good feedback from my attending and residents, and they are very well aware of the way I work. In fact I think they appreciate it because it shows them that I am interested, I enjoy what I am doing and I am learning.
I should not be afraid, nobody should be afraid. We should ALL be careful but thats a completely different topic. When I did my sub-I during my 4th year of medschool I rotated through the ICU of one of the largest university programs in the US. I saw dozens of central lines being placed by 3rd year residents and 1st year pulm-crit fellows. These otherwise mundane procedures took them easily 1h+ when they go smooth but I saw some central lines that took nearly 3 hours to place because they were terrified, sweating and hands shaking. I am talking about third year residents and fellows from a major, relatively prestigious program. They were very smart, brilliant actually, but they were also afraid. Fear did not help them. When I started my intern year, my first rotation was in the ICU. The third year resident placed a central line in 10mins, no sweat, no shakiness. Very confident. He was very careful, technique was excellent. After he did one on his own to show me he let me do the next. I felt very comfortable and fearless (a bit nervous I do admit, but no fear) since he was by my side and he was great. My hands did not shake, I did not sweat like a pig and I got my central line within 15-20mins on my first try without any hitch. Since then I have been able to do a few more that have also gone smooth. My ICU attending likes to say "if you have not caused a pneumothorax yet, you have not put enough central lines." One of the oldest pulmonologist of my program (he is in his 70s, and a brilliant doctor) was helping the same 3rd year resident that thought me to place the central line put a PICC line. The 3rd year resident started advancing the guide wire and says "I am finding resistance I am backing off", the Pulmonologist says "Let me try" he got the guide wire and caused a pneumothorax himself. It happens and I am aware it will eventually happen to me but this is why I need to learn because I have to be competent when it is my turn. The third year and even the 2nd year residents run the codes in my hospital. Attending are nearby or 1 call away and we all know it and that gives us confidence. But how am I supposed to run a code on my own next year if I am afraid today of ordering a CBC/X-ray/Tylenol? How can I possible tell the nurse to push epi, or shock someone or intubate someone if I cannot even decide on my own if I can give some over the counter cough medicine?
I wrote this mega-response because I was not sure if you misunderstood my degree of confidence or if you are truly advocating for residents to be scared. I do agree we have to be careful, not just residents/interns, but nurses and attending as well. But scared? No, I wholeheartedly disagree with you on that. First you won't learn, second you won't enjoy it and third you might actually kill more people being afraid.
- Joined
- May 1, 2010
- Messages
- 217
- Reaction score
- 198
So you recommend to instead be a frighten useless doctor instead? There is a is a fine line between being confident and careful and frighten and useless and I agree this line is kind of blurry, hard to see and I even doubt any doctor ever knows the difference. We all made mistakes and at one point or another we will all do some degree of harm. Most of the time knowingly (as part of a side effect) but sometimes also by mistake or even negligence. Fear, however is not the proper response.
Yes, I am only a 1st year intern but I am also and MD and I have to take responsibility and initiative otherwise the last 4 years were simply a waste of time.
I am not going to kill anyone for ordering a bunch of blood tests, X-rays, ultrasounds or EKG on my own. I am not going to kill anyone by ordering some cough medicine, Tylenol or some nebulizer inhalers. I am not going to kill someone by giving some fluids to someone that is not on CHF and that does not have some electrolyte imbalance such as hypo/hypernatremia, I am not going to kill someone for putting them NPO just because I am suspecting a weird diagnosis that might require a procedure.
Ofcourse I am careful with those medications that have more serious side effects. I am not going to be ordering heparin haphazardly without discussing it with the attending previously. But the only way to learn properly is to lose the training wheels and I think being comfortable with some simple decisions is definitely the first step. I have always discussed every single med I have given to my patients with attending and/or senior resident and asked feedback and if I did the correct thing. I do not necessarily discuss blood tests or imaging such as x-ray or ekg unless it comes back negative and I was not sure if I needed such test. So far I have got very good feedback from my attending and residents, and they are very well aware of the way I work. In fact I think they appreciate it because it shows them that I am interested, I enjoy what I am doing and I am learning.
I should not be afraid, nobody should be afraid. We should ALL be careful but thats a completely different topic. When I did my sub-I during my 4th year of medschool I rotated through the ICU of one of the largest university programs in the US. I saw dozens of central lines being placed by 3rd year residents and 1st year pulm-crit fellows. These otherwise mundane procedures took them easily 1h+ when they go smooth but I saw some central lines that took nearly 3 hours to place because they were terrified, sweating and hands shaking. I am talking about third year residents and fellows from a major, relatively prestigious program. They were very smart, brilliant actually, but they were also afraid. Fear did not help them. When I started my intern year, my first rotation was in the ICU. The third year resident placed a central line in 10mins, no sweat, no shakiness. Very confident. He was very careful, technique was excellent. After he did one on his own to show me he let me do the next. I felt very comfortable and fearless (a bit nervous I do admit, but no fear) since he was by my side and he was great. My hands did not shake, I did not sweat like a pig and I got my central line within 15-20mins on my first try without any hitch. Since then I have been able to do a few more that have also gone smooth. My ICU attending likes to say "if you have not caused a pneumothorax yet, you have not put enough central lines." One of the oldest pulmonologist of my program (he is in his 70s, and a brilliant doctor) was helping the same 3rd year resident that thought me to place the central line put a PICC line. The 3rd year resident started advancing the guide wire and says "I am finding resistance I am backing off", the Pulmonologist says "Let me try" he got the guide wire and caused a pneumothorax himself. It happens and I am aware it will eventually happen to me but this is why I need to learn because I have to be competent when it is my turn. The third year and even the 2nd year residents run the codes in my hospital. Attending are nearby or 1 call away and we all know it and that gives us confidence. But how am I supposed to run a code on my own next year if I am afraid today of ordering a CBC/X-ray/Tylenol? How can I possible tell the nurse to push epi, or shock someone or intubate someone if I cannot even decide on my own if I can give some over the counter cough medicine?
I wrote this mega-response because I was not sure if you misunderstood my degree of confidence or if you are truly advocating for residents to be scared. I do agree we have to be careful, not just residents/interns, but nurses and attending as well. But scared? No, I wholeheartedly disagree with you on that. First you won't learn, second you won't enjoy it and third you might actually kill more people being afraid.
A few things (I'm a PGY-3):
-It's ok, I don't think he was trying to personally attack your level of confidence. There is no one in the hospital who knows 100% what is going to happen with any given treatment and any given patient. If people did, we wouldn't need doctors anymore. When you become a PGY-2 or PGY-3, you'll be making tons of decisions without consulting with the attending first, and learning when to ask for help is an essential part of the residency experience.
-btw: no one cares how fast you can do a line or how good you can do a line. You can train literally anyone with enough practice to put in a line because it's a very technical skill, but you didn't go to med school to just learn to put in lines. You went to medical school to learn medical decision making and differential diagnoses, which is much more valuable in the long run than putting in lines (how many attendings know how to put in central lines?!)
To the OP:
Intern year was brutal. People always yelled at you for no good reason (consultants literally laughed in my face a couple of times even when I tried to present the case as a "team decision"), nurses were always harassing you with pages about glucose and dislodged IVs, and attendings always asked these esoteric questions that were impossible to answer after 5 hours of sleep. It gets A LOT better as juniors/seniors. I found the ICU calls to be pretty disastrous too later on but I found that as long as you keep everything in perspective you'll be fine (I mean, barring any clinical depression...etc. obvs). This too shall pass. THIS TOO SHALL PASS.
D
deleted547339
So you recommend to instead be a frighten useless doctor instead? There is a is a fine line between being confident and careful and frighten and useless and I agree this line is kind of blurry, hard to see and I even doubt any doctor ever knows the difference. We all made mistakes and at one point or another we will all do some degree of harm. Most of the time knowingly (as part of a side effect) but sometimes also by mistake or even negligence. Fear, however is not the proper response.
Yes, I am only a 1st year intern but I am also and MD and I have to take responsibility and initiative otherwise the last 4 years were simply a waste of time.
I am not going to kill anyone for ordering a bunch of blood tests, X-rays, ultrasounds or EKG on my own. I am not going to kill anyone by ordering some cough medicine, Tylenol or some nebulizer inhalers. I am not going to kill someone by giving some fluids to someone that is not on CHF and that does not have some electrolyte imbalance such as hypo/hypernatremia, I am not going to kill someone for putting them NPO just because I am suspecting a weird diagnosis that might require a procedure.
Ofcourse I am careful with those medications that have more serious side effects. I am not going to be ordering heparin haphazardly without discussing it with the attending previously. But the only way to learn properly is to lose the training wheels and I think being comfortable with some simple decisions is definitely the first step. I have always discussed every single med I have given to my patients with attending and/or senior resident and asked feedback and if I did the correct thing. I do not necessarily discuss blood tests or imaging such as x-ray or ekg unless it comes back negative and I was not sure if I needed such test. So far I have got very good feedback from my attending and residents, and they are very well aware of the way I work. In fact I think they appreciate it because it shows them that I am interested, I enjoy what I am doing and I am learning.
I should not be afraid, nobody should be afraid. We should ALL be careful but thats a completely different topic. When I did my sub-I during my 4th year of medschool I rotated through the ICU of one of the largest university programs in the US. I saw dozens of central lines being placed by 3rd year residents and 1st year pulm-crit fellows. These otherwise mundane procedures took them easily 1h+ when they go smooth but I saw some central lines that took nearly 3 hours to place because they were terrified, sweating and hands shaking. I am talking about third year residents and fellows from a major, relatively prestigious program. They were very smart, brilliant actually, but they were also afraid. Fear did not help them. When I started my intern year, my first rotation was in the ICU. The third year resident placed a central line in 10mins, no sweat, no shakiness. Very confident. He was very careful, technique was excellent. After he did one on his own to show me he let me do the next. I felt very comfortable and fearless (a bit nervous I do admit, but no fear) since he was by my side and he was great. My hands did not shake, I did not sweat like a pig and I got my central line within 15-20mins on my first try without any hitch. Since then I have been able to do a few more that have also gone smooth. My ICU attending likes to say "if you have not caused a pneumothorax yet, you have not put enough central lines." One of the oldest pulmonologist of my program (he is in his 70s, and a brilliant doctor) was helping the same 3rd year resident that thought me to place the central line put a PICC line. The 3rd year resident started advancing the guide wire and says "I am finding resistance I am backing off", the Pulmonologist says "Let me try" he got the guide wire and caused a pneumothorax himself. It happens and I am aware it will eventually happen to me but this is why I need to learn because I have to be competent when it is my turn. The third year and even the 2nd year residents run the codes in my hospital. Attending are nearby or 1 call away and we all know it and that gives us confidence. But how am I supposed to run a code on my own next year if I am afraid today of ordering a CBC/X-ray/Tylenol? How can I possible tell the nurse to push epi, or shock someone or intubate someone if I cannot even decide on my own if I can give some over the counter cough medicine?
I wrote this mega-response because I was not sure if you misunderstood my degree of confidence or if you are truly advocating for residents to be scared. I do agree we have to be careful, not just residents/interns, but nurses and attending as well. But scared? No, I wholeheartedly disagree with you on that. First you won't learn, second you won't enjoy it and third you might actually kill more people being afraid.
You should have a healthy fear of medicine. I didn't say you should be trembling in the corner crying, but you should be very afraid of hurting someone. It sounds like you're not. I'm sure you're convinced your right, but I hate having interns who think like you do on my service. Again, I'm not saying this to offend you, but interns (and essentially all residents) who aren't afraid are going to hurt people. They're going to make mistakes that kill people before they learn.
Your mistakes can take someone's life. And it's not always the "big" decisions. It can be making a patient NPO and then they miss a couple doses of lactulose which leads to AMS, then intubation, then PNA, then decompensated cirrhosis, then death. It can be the decision of leaving a line in an extra day when you didn't need it which can lead to bacteremia then septic shock then death. Little things add up. Sure, you're going to talk to your attending about lysing a PE or other "big ticket" items, but the little decisions can catch up to you and kill someone easier than you know. I'm not saying you're not a good intern, but it scares the hell out of me to hear someone who has been practicing medicine for 3 months say they're not afraid. They are the ones that hurt people because they "know what they're doing."
And if you think you're not going to kill anyone by ordering diagnostic tests, you're wrong. Ordering a trop on a patient that doesn't need it seem benign, but then that patient gets a stress that was positive, then a cath, then a hospital acquired infection. Order an unnecessary brain CTA and find an asymptomatic CNS aneurysm that nsgy feels the need to coil, a certain percent of them will end up neurologically devastated from unnecessary procedural misadventure. Also, if you think a guide wire dropped a lung, you don't understand how people cause a PTX placing a CVL or the attending did something horribly horribly wrong.
Everything in medicine has consequences. I know you are going to think that these scenarios are far fetched, but they're not. Everything in medicine has a downstream consequence. You are at the point in your career where you can't yet see the 10,000 foot view. Trust me when I say this. Be afraid - it's good for you and for your patients.
Edited for typo
Last edited by a moderator:
- Joined
- Sep 20, 2004
- Messages
- 6,007
- Reaction score
- 6,711
You are by far the type of intern that scares me...way to over confident and don't know what you don't know...So you recommend to instead be a frighten useless doctor instead? There is a is a fine line between being confident and careful and frighten and useless and I agree this line is kind of blurry, hard to see and I even doubt any doctor ever knows the difference. We all made mistakes and at one point or another we will all do some degree of harm. Most of the time knowingly (as part of a side effect) but sometimes also by mistake or even negligence. Fear, however is not the proper response.
Yes, I am only a 1st year intern but I am also and MD and I have to take responsibility and initiative otherwise the last 4 years were simply a waste of time.
I am not going to kill anyone for ordering a bunch of blood tests, X-rays, ultrasounds or EKG on my own. I am not going to kill anyone by ordering some cough medicine, Tylenol or some nebulizer inhalers. I am not going to kill someone by giving some fluids to someone that is not on CHF and that does not have some electrolyte imbalance such as hypo/hypernatremia, I am not going to kill someone for putting them NPO just because I am suspecting a weird diagnosis that might require a procedure.
Ofcourse I am careful with those medications that have more serious side effects. I am not going to be ordering heparin haphazardly without discussing it with the attending previously. But the only way to learn properly is to lose the training wheels and I think being comfortable with some simple decisions is definitely the first step. I have always discussed every single med I have given to my patients with attending and/or senior resident and asked feedback and if I did the correct thing. I do not necessarily discuss blood tests or imaging such as x-ray or ekg unless it comes back negative and I was not sure if I needed such test. So far I have got very good feedback from my attending and residents, and they are very well aware of the way I work. In fact I think they appreciate it because it shows them that I am interested, I enjoy what I am doing and I am learning.
I should not be afraid, nobody should be afraid. We should ALL be careful but thats a completely different topic. When I did my sub-I during my 4th year of medschool I rotated through the ICU of one of the largest university programs in the US. I saw dozens of central lines being placed by 3rd year residents and 1st year pulm-crit fellows. These otherwise mundane procedures took them easily 1h+ when they go smooth but I saw some central lines that took nearly 3 hours to place because they were terrified, sweating and hands shaking. I am talking about third year residents and fellows from a major, relatively prestigious program. They were very smart, brilliant actually, but they were also afraid. Fear did not help them. When I started my intern year, my first rotation was in the ICU. The third year resident placed a central line in 10mins, no sweat, no shakiness. Very confident. He was very careful, technique was excellent. After he did one on his own to show me he let me do the next. I felt very comfortable and fearless (a bit nervous I do admit, but no fear) since he was by my side and he was great. My hands did not shake, I did not sweat like a pig and I got my central line within 15-20mins on my first try without any hitch. Since then I have been able to do a few more that have also gone smooth. My ICU attending likes to say "if you have not caused a pneumothorax yet, you have not put enough central lines." One of the oldest pulmonologist of my program (he is in his 70s, and a brilliant doctor) was helping the same 3rd year resident that thought me to place the central line put a PICC line. The 3rd year resident started advancing the guide wire and says "I am finding resistance I am backing off", the Pulmonologist says "Let me try" he got the guide wire and caused a pneumothorax himself. It happens and I am aware it will eventually happen to me but this is why I need to learn because I have to be competent when it is my turn. The third year and even the 2nd year residents run the codes in my hospital. Attending are nearby or 1 call away and we all know it and that gives us confidence. But how am I supposed to run a code on my own next year if I am afraid today of ordering a CBC/X-ray/Tylenol? How can I possible tell the nurse to push epi, or shock someone or intubate someone if I cannot even decide on my own if I can give some over the counter cough medicine?
I wrote this mega-response because I was not sure if you misunderstood my degree of confidence or if you are truly advocating for residents to be scared. I do agree we have to be careful, not just residents/interns, but nurses and attending as well. But scared? No, I wholeheartedly disagree with you on that. First you won't learn, second you won't enjoy it and third you might actually kill more people being afraid.
- Joined
- Sep 14, 2013
- Messages
- 410
- Reaction score
- 196
You are by far the type of intern that scares me...way to over confident and don't know what you don't know...
This's normal for a few interns. It will wear off quickly with the first couple of deadly mistakes
- Joined
- Jan 2, 2014
- Messages
- 11,384
- Reaction score
- 24,014
I gotta agree with the other residents and fellows here. You definitely need to slow things down. I've seen patients become unstable from all the blood draws they've gotten as well as fluid overload from residents not paying attention to total fluid balance. Ordering useless tests can discover incidentalomas that lead to further testing and a downward spiral into the icu, then the morgue.
There is no such thing as healthy fear. Fear should be like the engine light in your car. It pops once, you acknowledge it and put it aside until such time it is appropriate to have it check. When I got something I am not 100% sure I don't freak out. If possible I read and make a judgment if I can take action on my own and consult it later with the rest of the team if required. If all I do is rely on information between the nurse calling me and my attending or senior, eventually the nurse will get tired of calling me and will go straight over my head every single time. This has happened to a couple of my co-interns already. This is detrimental to my learning, this keeps me out of the loop so I don't know whats going on with my patients because the attending is doing stuff without my knowledge and eventually affects the quality of care my patient receives. Not to mention it is annoying for me, the nurse and the attending. I made it clear in my first post that I would always discuss every medication, and most test I order w/ my supervisor team. I simply don't have to ask permission for every single step i take.You should have a healthy fear of medicine. I didn't say you should be trembling in the corner crying, but you should be very afraid of hurting someone. It sounds like you're not. I'm sure you're convinced your right, but I hate having interns who think like you do on my service. Again, I'm not saying this to offend you, but interns (and essentially all residents) who aren't afraid are going to hurt people. They're going to make mistakes that kill people before they learn.
Your mistakes can take someone's life. And it's not always the "big" decisions. It can be making a patient NPO and then they miss a couple doses of lactulose which leads to AMS, then intubation, then PNA, then decompensated cirrhosis, then death. It can be the decision of leaving a line in an extra day when you didn't need it which can lead to bacteremia then septic shock then death. Little things add up. Sure, you're going to talk to your attending about lysing a PE or other "big ticket" items, but the little decisions can catch up to you and kill someone easier than you know. I'm not saying you're not a good intern, but it scares the hell out of me to hear someone who has been practicing medicine for 3 months say they're not afraid. They are the ones that hurt people because they "know what they're doing."
And if you think you're not going to kill anyone by ordering diagnostic tests, you're wrong. Ordering a trop on a patient that doesn't need it seem benign, but then that patient gets a stress that was positive, then a cath, then a hospital acquired infection. Order an unnecessary brain CTA and find an asymptomatic CNS aneurysm that nsgy feels the need to coil, a certain percent of them will end up neurologically devastated from unnecessary procedural misadventure. Also, if you think a guide wire dropped a lung, you don't understand how people cause a PTX placing a CVL or the attending did something horribly horribly wrong.
Everything in medicine has consequences. I know you are going to think that these scenarios are far fetched, but they're not. Everything in medicine has a downstream consequence. You are at the point in your career where you can't yet see the 10,000 foot view. Trust me when I say this. Be afraid - it's good for you and for your patients.
Edited for typo
You say, "Your mistakes can take someone's life. And it's not always the "big" decisions." but guess what. Everyone's mistake can take someone's life. Not just interns or residents or attendings but also nurses, ancillary staff or every a random person from the street. Every single doctor that has ever practice has and will continue to cause some harm to a few of their patients and that's a fact. Hopefully, most of that harm is mitigated by being identified early and addressed. I am going to make mistakes through my career that is a fact, as it is a fact you have made your owns already and will continue to make them until you die. But guess what, this is the safest time in all my career where a mistake I can make will be mitigated. My mistake can now be caught by my senior and/or my attending. If I am ever going to make a mistake that could potentially harm someone to the point of putting their life at risk, this is the best time for it. Hopefully, it will never happen.
In the same example, you gave about ordering a troponin that was not necessary at all. In this hypothetical example, maybe I was wrong to order the test to begin with, fine I'll take that. But guess what, for the patient to go to cath and have the complication that you mentioned that test would have to be analyzed by my senior, my attending, the cardiologist and/or the interventional cardiologist even before the patient goes for the procedure. If the test was inappropriate each and every one of those people should have pointed it out, give a reasonable explanation (e.g. maybe trops elevated because demand ischemia, or because patient is in ESRD or because of septic cardiomyopathy or simply because the test was a false positive or the guy in the lab changed the test tube my mistake.) It makes absolutely no sense for you to blame the intern for a poor outcome that happened because of such chain of command. Sure, I would have to hold some responsibility, I ordered the useless test after all. But nothing, NOTHING compared to the mistakes of all the more experienced physicians that acted on a test that was not appropriate, to begin with.
Like I said before, this is the time in my training that if I make a mistake, it will likely get caught in time and harm will be mitigated.
Don't come to me with that double standard of ordering unnecessary tests or unnecessary treatment. I am tired of telling my clinic patients that I will not give them antibiotics for a sore throat so that my attending later agrees that I am in the right because the patient does not need an antibiotic, but to go ahead and give it to them "to make them feel better". No intern will ever get close to ordering as many useless test as the average ER physician does in a month of work. Half the patients that come into the ED get a set of troponins and d-dimmers even for a stuffy nose or vancomycin and ceftriaxone for an infected pimple. This is not a problem limited to my current hospital, I have rotated as a medstudent in half a dozen hospitals (a few of them respectable university institutions) where this is common occurrence. So while I agree with you in principle that we should be conscious about what we order, the fact of the matter is that neither of us actually practice what we preach. Ideally, I would like to learn the correct tests and the correct way to tell my patients "I will not give you ABX for your stuffy nose" which brings me back to square one, the only way to learn includes making mistakes. And this is the safest place for anyone to make such mistakes before a long career where you could potentially make a mistake that will be lethal.
My attendings rarely if ever have to write progress/consult notes because the intern does that, my senior residents seldom has to write notes himself (unless other interns are on their day off). Part of their job is to supervise my work, read my notes and review my orders and discuss if I made any mistake. The "afraid" intern can very well put the wrong order by mistake, happens all the time (and I'd argue that being scared predisposes you to make such mistake by being nervous) and those in supervising roles also must catch those mistakes.
I am sorry, but being one of those hospitalists that don't even see their patient that they admit and put consult on cardiology/pulmonology/ID for a CAP and sit back and relax while the consultants do the work is not my ideal job.
Honestly, I don't know what to say other than advice you to check the uptodate page on PICC lines and Central lines for complications. You do realize the lungs are those large things that usually sit to both sides of the SVC right?Also, if you think a guide wire dropped a lung, you don't understand how people cause a PTX placing a CVL or the attending did something horribly horribly wrong.
I'll give you a clue. After all PICC/CVL every patient get a CXR. You never seen this practice before? What did you think that CXR was for? check for pneumonia? Correct placement is just a minor reason. You can technically use a central line right away without CXR if you confirm it is placed in the venous system (e.g. you get venous return rather than arterial squirt or air/dry tap). You need the CXR to make sure you did not pop a lung. And yes the pneumothorax rate is relatively small (~1%) but that is still quite common. For instance, I estimate my hospital probably places somewhere between 5-10 daily. So on average, in my hospital, I would expect to see 1 pneumothorax every two weeks or so. My ICU attendings have probably done thousands during their careers, so I was not surprised to hear most of them have caused a few dozen through their career.
Haha! According to TimesNewRoman fear is healthy for medicine so I guess we would make the perfect team then.You are by far the type of intern that scares me...way to over confident and don't know what you don't know...
Sorry if I take your feedback with a grain of salt. The feedback I do really care is that of my senior residents and my attendings that work with me all day long and see my competence (and lack of it) and my thinking process and decision making. I disagree with being afraid, period. I agree with being cautious, and perhaps there is some kind of miscommunication but I am a cautious intern. I am the kind of intern that call a discharged patient to ask how they are doing after being discharged because a blood culture came back positive. I am the kind of intern that check the labs/med orders I put for my patients prior to leaving the hospital and then prior to going to bed from home.
Last edited:
D
deleted547339
There is no such thing as healthy fear. Fear should be like the engine light in your car. It pops once, you acknowledge it and put it aside until such time it is appropriate to have it check. When I got something I am not 100% sure I don't freak out. If possible I read and make a judgment if I can take action on my own and consult it later with the rest of the team if required. If all I do is rely on information between the nurse calling me and my attending or senior, eventually the nurse will get tired of calling me and will go straight over my head every single time. This has happened to a couple of my co-interns already. This is detrimental to my learning, this keeps me out of the loop so I don't know whats going on with my patients because the attending is doing stuff without my knowledge and eventually affects the quality of care my patient receives. Not to mention it is annoying for me, the nurse and the attending. I made it clear in my first post that I would always discuss every medication, and most test I order w/ my supervisor team. I simply don't have to ask permission for every single step i take.
You say, "Your mistakes can take someone's life. And it's not always the "big" decisions." but guess what. Everyone's mistake can take someone's life. Not just interns or residents or attendings but also nurses, ancillary staff or every a random person from the street. Every single doctor that has ever practice has and will continue to cause some harm to a few of their patients and that's a fact. Hopefully, most of that harm is mitigated by being identified early and addressed. I am going to make mistakes through my career that is a fact, as it is a fact you have made your owns already and will continue to make them until you die. But guess what, this is the safest time in all my career where a mistake I can make will be mitigated. My mistake can now be caught by my senior and/or my attending. If I am ever going to make a mistake that could potentially harm someone to the point of putting their life at risk, this is the best time for it. Hopefully, it will never happen.
In the same example, you gave about ordering a troponin that was not necessary at all. In this hypothetical example, maybe I was wrong to order the test to begin with, fine I'll take that. But guess what, for the patient to go to cath and have the complication that you mentioned that test would have to be analyzed by my senior, my attending, the cardiologist and/or the interventional cardiologist even before the patient goes for the procedure. If the test was inappropriate each and every one of those people should have pointed it out, give a reasonable explanation (e.g. maybe trops elevated because demand ischemia, or because patient is in ESRD or because of septic cardiomyopathy or simply because the test was a false positive or the guy in the lab changed the test tube my mistake.) It makes absolutely no sense for you to blame the intern for a poor outcome that happened because of such chain of command. Sure, I would have to hold some responsibility, I ordered the useless test after all. But nothing, NOTHING compared to the mistakes of all the more experienced physicians that acted on a test that was not appropriate, to begin with.
Like I said before, this is the time in my training that if I make a mistake, it will likely get caught in time and harm will be mitigated.
Don't come to me with that double standard of ordering unnecessary tests or unnecessary treatment. I am tired of telling my clinic patients that I will not give them antibiotics for a sore throat so that my attending later agrees that I am in the right because the patient does not need an antibiotic, but to go ahead and give it to them "to make them feel better". No intern will ever get close to ordering as many useless test as the average ER physician does in a month of work. Half the patients that come into the ED get a set of troponins and d-dimmers even for a stuffy nose or vancomycin and ceftriaxone for an infected pimple. This is not a problem limited to my current hospital, I have rotated as a medstudent in half a dozen hospitals (a few of them respectable university institutions) where this is common occurrence. So while I agree with you in principle that we should be conscious about what we order, the fact of the matter is that neither of us actually practice what we preach. Ideally, I would like to learn the correct tests and the correct way to tell my patients "I will not give you ABX for your stuffy nose" which brings me back to square one, the only way to learn includes making mistakes. And this is the safest place for anyone to make such mistakes before a long career where you could potentially make a mistake that will be lethal.
My attendings rarely if ever have to write progress/consult notes because the intern does that, my senior residents seldom has to write notes himself (unless other interns are on their day off). Part of their job is to supervise my work, read my notes and review my orders and discuss if I made any mistake. The "afraid" intern can very well put the wrong order by mistake, happens all the time (and I'd argue that being scared predisposes you to make such mistake by being nervous) and those in supervising roles also must catch those mistakes.
I am sorry, but being one of those hospitalists that don't even see their patient that they admit and put consult on cardiology/pulmonology/ID for a CAP and sit back and relax while the consultants do the work is not my ideal job.
Honestly, I don't know what to say other than advice you to check the uptodate page on PICC lines and Central lines for complications. You do realize the lungs are those large things that usually sit to both sides of the SVC right?
I'll give you a clue. After all PICC/CVL every patient get a CXR. You never seen this practice before? What did you think that CXR was for? check for pneumonia? Correct placement is just a minor reason. You can technically use a central line right away without CXR if you confirm it is placed in the venous system (e.g. you get venous return rather than arterial squirt or air/dry tap). You need the CXR to make sure you did not pop a lung. And yes the pneumothorax rate is relatively small (~1%) but that is still quite common. For instance, I estimate my hospital probably places somewhere between 5-10 daily. So on average, in my hospital, I would expect to see 1 pneumothorax every two weeks or so. My ICU attendings have probably done thousands during their careers, so I was not surprised to hear most of them have caused a few dozen through their career.
Haha! According to TimesNewRoman fear is healthy for medicine so I guess we would make the perfect team then.
Sorry if I take your feedback with a grain of salt. The feedback I do really care is that of my senior residents and my attendings that work with me all day long and see my competence (and lack of it) and my thinking process and decision making. I disagree with being afraid, period. I agree with being cautious, and perhaps there is some kind of miscommunication but I am a cautious intern. I am the kind of intern that call a discharged patient to ask how they are doing after being discharged because a blood culture came back positive. I am the kind of intern that check the labs/med orders I put for my patients prior to leaving the hospital and then prior to going to bed from home.
I'm glad in being a doctor for 3 months you've already figured out how to practice emergency medicine and hospitalist medicine better than a board certified doctor and don't need to ever take any advice from people your senior. I've learned not to argue with fools, and your post clearly demonstrates that you lack insight. I was trying to give you somewhat constructive advice, but you would rather be proud than respect the profession. Without a healthy fear, you will harm the patients that have entrusted their lives to you. Although it seems you lack the insight to appreciate this, at some point in the next year or two, you will have an 'ah-ha' moment after you kill someone.
The only thing worth clarifying in response to your idiotic, pejorative statement about placing central lines was that you literally have no idea what I was saying about the central line. You can't drop a lung with a guidewire, you drop it with the needle. Forcing a guide wire can cause a vascular injury, but you aren't going to cause a pulmonary injury without causing catastrophic vascular rupture, You are either lying about your anecdote, or you're just really dumb. You said your faculty dropped a lung by advancing the guide wire while placing a picc....you are literally making stuff up to prove a point to someone on the internet. You sound like an idiot - you should stop.
Last edited by a moderator:
- Joined
- Sep 20, 2004
- Messages
- 6,007
- Reaction score
- 6,711
There is no such thing as healthy fear. Fear should be like the engine light in your car. It pops once, you acknowledge it and put it aside until such time it is appropriate to have it check. When I got something I am not 100% sure I don't freak out. If possible I read and make a judgment if I can take action on my own and consult it later with the rest of the team if required. If all I do is rely on information between the nurse calling me and my attending or senior, eventually the nurse will get tired of calling me and will go straight over my head every single time. This has happened to a couple of my co-interns already. This is detrimental to my learning, this keeps me out of the loop so I don't know whats going on with my patients because the attending is doing stuff without my knowledge and eventually affects the quality of care my patient receives. Not to mention it is annoying for me, the nurse and the attending. I made it clear in my first post that I would always discuss every medication, and most test I order w/ my supervisor team. I simply don't have to ask permission for every single step i take.
You say, "Your mistakes can take someone's life. And it's not always the "big" decisions." but guess what. Everyone's mistake can take someone's life. Not just interns or residents or attendings but also nurses, ancillary staff or every a random person from the street. Every single doctor that has ever practice has and will continue to cause some harm to a few of their patients and that's a fact. Hopefully, most of that harm is mitigated by being identified early and addressed. I am going to make mistakes through my career that is a fact, as it is a fact you have made your owns already and will continue to make them until you die. But guess what, this is the safest time in all my career where a mistake I can make will be mitigated. My mistake can now be caught by my senior and/or my attending. If I am ever going to make a mistake that could potentially harm someone to the point of putting their life at risk, this is the best time for it. Hopefully, it will never happen.
In the same example, you gave about ordering a troponin that was not necessary at all. In this hypothetical example, maybe I was wrong to order the test to begin with, fine I'll take that. But guess what, for the patient to go to cath and have the complication that you mentioned that test would have to be analyzed by my senior, my attending, the cardiologist and/or the interventional cardiologist even before the patient goes for the procedure. If the test was inappropriate each and every one of those people should have pointed it out, give a reasonable explanation (e.g. maybe trops elevated because demand ischemia, or because patient is in ESRD or because of septic cardiomyopathy or simply because the test was a false positive or the guy in the lab changed the test tube my mistake.) It makes absolutely no sense for you to blame the intern for a poor outcome that happened because of such chain of command. Sure, I would have to hold some responsibility, I ordered the useless test after all. But nothing, NOTHING compared to the mistakes of all the more experienced physicians that acted on a test that was not appropriate, to begin with.
Like I said before, this is the time in my training that if I make a mistake, it will likely get caught in time and harm will be mitigated.
Don't come to me with that double standard of ordering unnecessary tests or unnecessary treatment. I am tired of telling my clinic patients that I will not give them antibiotics for a sore throat so that my attending later agrees that I am in the right because the patient does not need an antibiotic, but to go ahead and give it to them "to make them feel better". No intern will ever get close to ordering as many useless test as the average ER physician does in a month of work. Half the patients that come into the ED get a set of troponins and d-dimmers even for a stuffy nose or vancomycin and ceftriaxone for an infected pimple. This is not a problem limited to my current hospital, I have rotated as a medstudent in half a dozen hospitals (a few of them respectable university institutions) where this is common occurrence. So while I agree with you in principle that we should be conscious about what we order, the fact of the matter is that neither of us actually practice what we preach. Ideally, I would like to learn the correct tests and the correct way to tell my patients "I will not give you ABX for your stuffy nose" which brings me back to square one, the only way to learn includes making mistakes. And this is the safest place for anyone to make such mistakes before a long career where you could potentially make a mistake that will be lethal.
My attendings rarely if ever have to write progress/consult notes because the intern does that, my senior residents seldom has to write notes himself (unless other interns are on their day off). Part of their job is to supervise my work, read my notes and review my orders and discuss if I made any mistake. The "afraid" intern can very well put the wrong order by mistake, happens all the time (and I'd argue that being scared predisposes you to make such mistake by being nervous) and those in supervising roles also must catch those mistakes.
I am sorry, but being one of those hospitalists that don't even see their patient that they admit and put consult on cardiology/pulmonology/ID for a CAP and sit back and relax while the consultants do the work is not my ideal job.
Honestly, I don't know what to say other than advice you to check the uptodate page on PICC lines and Central lines for complications. You do realize the lungs are those large things that usually sit to both sides of the SVC right?
I'll give you a clue. After all PICC/CVL every patient get a CXR. You never seen this practice before? What did you think that CXR was for? check for pneumonia? Correct placement is just a minor reason. You can technically use a central line right away without CXR if you confirm it is placed in the venous system (e.g. you get venous return rather than arterial squirt or air/dry tap). You need the CXR to make sure you did not pop a lung. And yes the pneumothorax rate is relatively small (~1%) but that is still quite common. For instance, I estimate my hospital probably places somewhere between 5-10 daily. So on average, in my hospital, I would expect to see 1 pneumothorax every two weeks or so. My ICU attendings have probably done thousands during their careers, so I was not surprised to hear most of them have caused a few dozen through their career.
Haha! According to TimesNewRoman fear is healthy for medicine so I guess we would make the perfect team then.
Sorry if I take your feedback with a grain of salt. The feedback I do really care is that of my senior residents and my attendings that work with me all day long and see my competence (and lack of it) and my thinking process and decision making. I disagree with being afraid, period. I agree with being cautious, and perhaps there is some kind of miscommunication but I am a cautious intern. I am the kind of intern that call a discharged patient to ask how they are doing after being discharged because a blood culture came back positive. I am the kind of intern that check the labs/med orders I put for my patients prior to leaving the hospital and then prior to going to bed from home.
trust me,you would not have wanted me as your senior or your attending.
- Joined
- May 1, 2010
- Messages
- 217
- Reaction score
- 198
I am tired of telling my clinic patients that I will not give them antibiotics for a sore throat so that my attending later agrees that I am in the right because the patient does not need an antibiotic, but to go ahead and give it to them "to make them feel better". No intern will ever get close to ordering as many useless test as the average ER physician does in a month of work. Half the patients that come into the ED get a set of troponins and d-dimmers even for a stuffy nose or vancomycin and ceftriaxone for an infected pimple. This is not a problem limited to my current hospital, I have rotated as a medstudent in half a dozen hospitals (a few of them respectable university institutions) where this is common occurrence. So while I agree with you in principle that we should be conscious about what we order, the fact of the matter is that neither of us actually practice what we preach.
I'm sorry, at first I was giving you the benefit of the doubt but...
1. What is your point about sore throats and abx? If something is indicated then it is indicated, if it's not then it's not. You should be firm about this regardless of what other people do. But be sure about your facts first, because what's worse than an idiot is an idiot who refuses to admit he's wrong.
2. Internal medicine and ED are totally different fields with very different lines of thinking. To compare the two in terms of diagnostics and treatments on equal footing reflects how little you know about clinical decision making in the hospital.
3. I have never seen anyone give ceftriaxone for an infected pimple, period. You need to work at better hospitals if that's what you're seeing, or stop making up stuff.
- Joined
- Sep 19, 2011
- Messages
- 4,832
- Reaction score
- 14,370
I'm glad in being a doctor for 3 months you've already figured out how to practice emergency medicine and hospitalist medicine better than a board certified doctor and don't need to ever take any advice from people your senior. I've learned not to argue with fools, and your post clearly demonstrates that you lack insight. I was trying to give you somewhat constructive advice, but you would rather be proud than respect the profession. Without a healthy fear, you will harm the patients that have entrusted their lives to you. Although it seems you lack the insight to appreciate this, at some point in the next year or two, you will have an 'ah-ha' moment after you kill someone.
The only thing worth clarifying in response to your idiotic, pejorative statement about placing central lines was that you literally have no idea what I was saying about the central line. You can't drop a lung with a guidewire, you drop it with the needle. Forcing a guide wire can cause a vascular injury, but you aren't going to cause a pulmonary injury without causing catastrophic vascular rupture, You are either lying about your anecdote, or you're just really dumb. You said your faculty dropped a lung by advancing the guide wire while placing a picc....you are literally making stuff up to prove a point to someone on the internet. You sound like an idiot - you should stop.
Just to clarify the clarification (not that I don't agree with your points) because I can't help myself... As the person responsible for cleaning up line placement ****-ups... The majority of central line complications occur from mis-use of the needle, followed by the dilators, followed by wires. Pneumothorax is relatively minor compared to vessel injury.
A few other things... The 1-2% complication rate is bull****. It is more like 1-25% given the massive variability among practitioners. By FAR the worst are people that think they know what they are doing, but really don't have much training in central access. I trust my current fourth year medical student more than I trust several staff physicians at least with placing a central line.
Similar threads
- Replies
- 21
- Views
- 2K
- Replies
- 3
- Views
- 615
- Replies
- 12
- Views
- 3K
- Replies
- 7
- Views
- 1K