Says you and ASTRO. NCCN guidelines still say 25 fractions is a standard. It still has a much greater representation in the randomized literature in terms of patient number versus hypofx (perhaps 100 to one?), and always will I suppose. And don't get me wrong: I'm acutely, profoundly aware of all the data. I just disagree that the old tried and true standard is no longer the standard, or a standard. People (invariably younger ones!) who think it's no longer the standard have perhaps succumbed to the
anxiety of influence.
Of course... 30Gy/5fx will work. As I said,
even giving zero gray works. But in alpha/beta's continuing triumphs (
sorry Eli), we have shown that 50/25 equals 42.5/16 and 39/13. We've shown it clinically. If we assume a/b=3 for breast cancer, then 50/25=83Gy3, 42.5/16=80Gy3, and 39/13=78Gy3 (and this is why 39/13 has shown best cosmesis?).
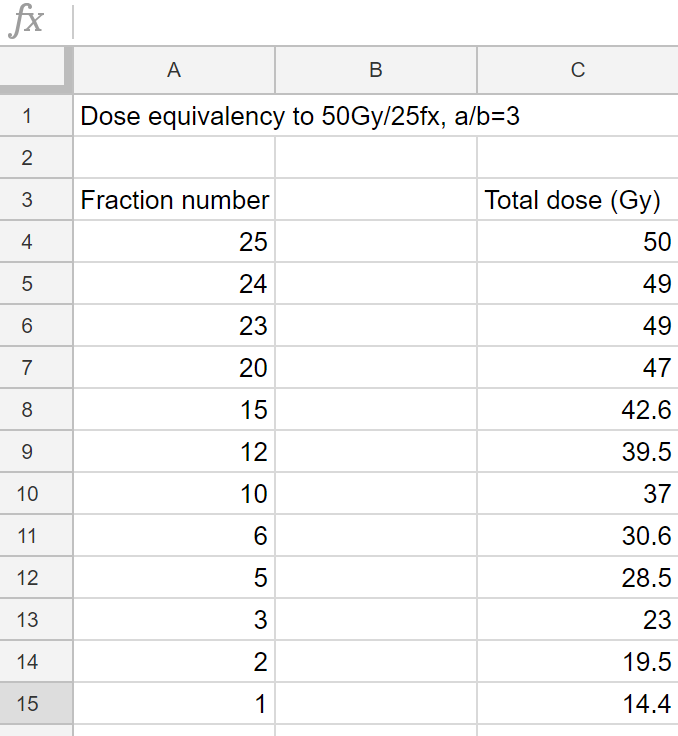
Also we showed 40/15=75Gy3 is OK for partial breast. Knowing all that, you can do something like this:
30/5 will be a boring trial for breast CA (but I guess if you're an academic, doing a trial you know will be good is the best trial to do). We know it will work (
like someone said above). We know it will be totally equivalent to 50/25 or 42.5/16 or 40/15 partial breast. (But will it be "true SBRT?") We have a professional society (ASTRO) where people published articles saying IMRT was superior in breast cancer, but the society came out and said the people publishing about breast IMRT weren't doing "true" IMRT. Anyone doing SBRT for breast is at risk for the professional society coming out and saying one shouldn't bill SBRT for breast, yes?
Doing five fractions or less is the only way to get SBRT paid. Anything over 5 fractions: not SBRT. It would be better from a patient/societal standpoint, perhaps, to do a six-fraction breast trial vs a five-fraction breast trial. Just to bill a patient and insurance thousands and thousands of more dollars for doing just one less treatment (ie five vs six fractions) seems "attackable." Like some might say it's "inappropriate" (I hate that word) to bill SBRT for five fractions when you could do same exact treatment as 3D "SBRT lite" for six fractions? Maybe even best would be ~14.4 Gy in one fraction billed as 3D per the math (again, see spreadsheet above). One fraction would be cheapest! If we could show 30/5 is good for breast (and like I said, that trial is destined for a resounding non-failure), we could all easily say 30/6 (impossible to bill as SBRT) is good for breast. Certainly 30/6 would be WAY cheaper than 30/5.
As things are going, and I am not saying this with irony believe it or not, we will likely one day show (and profess) that for tumors whose a/b is 3 or less, a single fraction is the optimal approach. This is rad onc in 2018 thanks to Evicore (and ASTRO): the best rad onc trials are the ones where really all we're testing is if cheap, or quick, tx is OK. Something tells me as we go
really quick, some people are trying to scoot cheap aside. They will find in time that they can not.