- Joined
- Nov 21, 1998
- Messages
- 12,564
- Reaction score
- 6,955
ASIPPNewsMast
Final CMS Payment Rules
for Interventional Pain Physicians
In-Office, ASC, and HOPD Settings
CMS released all 3 payment rules on November 1, 2019. These rules have multiplepdates including:
1. Interventional -Specific News
The good news, bad news, and ugly news continue to play out in the final rule, along with some errors, which we thought would be corrected, but have not.
1.1 Physician Payment Schedule
The CY 2020 Medicare Physician Fee Schedule (PFS) conversion factor is $36.09 (0.14% increase from CY 2019 conversion factor, was $36.04).
Overall, the cuts proposed for intercostal nerve blocks, vagus nerve block, ilioinguinal, and iliohypogastric nerve block reductions continue.
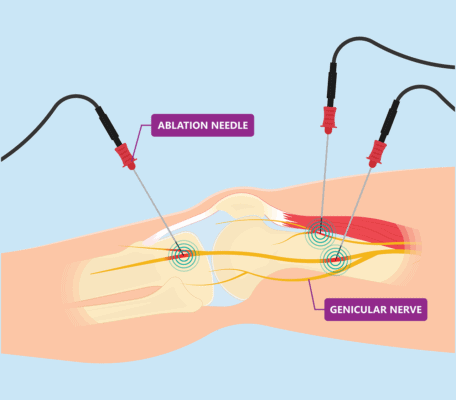
Some of the highlights include an increase in payment rates for sacroiliac joint nerve blocks, genicular nerve radiofrequency neurotomy, and sacroiliac joint nerve radiofreqency neurotomy, when performed in an office setting.
Sacroiliac joint fusion when performed in any setting.
1.2 Hospital Outpatient Department
Hospital outpatient departments continue to reap benefits wherein they are being paid double the payment of ASCs.
Of note is that interspinous stabilization device or prosthesis continues to face a 22.7% decline, along with a 62.3% decline for disc decompression.
New injection codes and genicular nerve block codes are paid appropriately in a hospital setting.
1.3 Ambulatory Surgery Centers
ASCs are paid less than 50% of hospital departments for non-implantables.
Most importantly, CMS has miscalculated payments for genicular nerve blocks and genicular radiofrequency neurotomy, which is 20% of the hospital payments instead of 50% of HOPD rate.
Multiple changes performed in the past have been preserved.
Interspinous prosthesis continues to face a 21.6% cut compared to 2019.
64421 (Injection(s), anesthetic agent(s) and/or steroid; intercostal nerves, each additional level - converted to add-on code - No payments in ASC & HOPD settings).
Disc decompression faces a significant cut of 59%.
Trigeminal nerve blocks, greater occipital nerve block, vagus nerve block, and suprascapular nerve block continue to face significant cuts.
2. Site-neutral Payments
CMS will finish phasing in a policy adapted in 2018 to make payments for clinic visits site neutral by reducing payments for hospital outpatient clinic visits provided at off campus provider-based departments. Medicare will pay doctors the same amount for a basic visit, whether it takes place in a hospital outpatient facility or a regular doctor's office.
3. Evaluation and Management, Coding, and Payment
The final sets separate payment rates for all 5 levels of coding for evaluation and management visits. The changes will be implemented on January 1, 2021.
4. Medical Record Documentation
The final rule allows physicians, physician assistants, and advanced practice registered nurses to review and verify information in a patient's medical record that is entered by other clinicians, rather than re-entering the information.
5. Telehealth Services
CMS will add a set of codes that describe a bundled episode of care for treatment of opioid use disorders, to the list of telehealth services covered by Medicare.
6. MIPS - 2020 performance period
45 points is the performance threshold (increased 15 points from PY 2019)
The Quality performance category is weighted at 45% (no change from PY 2019)
The Cost performance category is weighted at 15% (no change from PY 2019)
The Promoting Interoperability performance category is weighted at 25% (no change from PY 2019)
Here are the links Payment rates for major IPM codes:
Physician Fee Schedule:
https://www.asipp.org/Fee Schedules/2020PhysicianFinalRates.pdf
ASC Fee Schedule:
https://www.asipp.org/Fee Schedules/2020ASCFinalRates.pdf
HOPD Fee Schedule:
The following is important information on the newly released 2020 final payment rules. ASIPP and SIPMS will be sending comment letters to CMS. You may also send comment letters to them on these payment rules no later than 5 p.m. EST on December 2, 2019.
Final CMS Payment Rules
for Interventional Pain Physicians
In-Office, ASC, and HOPD Settings
CMS released all 3 payment rules on November 1, 2019. These rules have multiplepdates including:
1. Interventional -Specific News
The good news, bad news, and ugly news continue to play out in the final rule, along with some errors, which we thought would be corrected, but have not.
1.1 Physician Payment Schedule
The CY 2020 Medicare Physician Fee Schedule (PFS) conversion factor is $36.09 (0.14% increase from CY 2019 conversion factor, was $36.04).
Overall, the cuts proposed for intercostal nerve blocks, vagus nerve block, ilioinguinal, and iliohypogastric nerve block reductions continue.
Some of the highlights include an increase in payment rates for sacroiliac joint nerve blocks, genicular nerve radiofrequency neurotomy, and sacroiliac joint nerve radiofreqency neurotomy, when performed in an office setting.
Sacroiliac joint fusion when performed in any setting.
1.2 Hospital Outpatient Department
Hospital outpatient departments continue to reap benefits wherein they are being paid double the payment of ASCs.
Of note is that interspinous stabilization device or prosthesis continues to face a 22.7% decline, along with a 62.3% decline for disc decompression.
New injection codes and genicular nerve block codes are paid appropriately in a hospital setting.
1.3 Ambulatory Surgery Centers
ASCs are paid less than 50% of hospital departments for non-implantables.
Most importantly, CMS has miscalculated payments for genicular nerve blocks and genicular radiofrequency neurotomy, which is 20% of the hospital payments instead of 50% of HOPD rate.
Multiple changes performed in the past have been preserved.
Interspinous prosthesis continues to face a 21.6% cut compared to 2019.
64421 (Injection(s), anesthetic agent(s) and/or steroid; intercostal nerves, each additional level - converted to add-on code - No payments in ASC & HOPD settings).
Disc decompression faces a significant cut of 59%.
Trigeminal nerve blocks, greater occipital nerve block, vagus nerve block, and suprascapular nerve block continue to face significant cuts.
2. Site-neutral Payments
CMS will finish phasing in a policy adapted in 2018 to make payments for clinic visits site neutral by reducing payments for hospital outpatient clinic visits provided at off campus provider-based departments. Medicare will pay doctors the same amount for a basic visit, whether it takes place in a hospital outpatient facility or a regular doctor's office.
3. Evaluation and Management, Coding, and Payment
The final sets separate payment rates for all 5 levels of coding for evaluation and management visits. The changes will be implemented on January 1, 2021.
4. Medical Record Documentation
The final rule allows physicians, physician assistants, and advanced practice registered nurses to review and verify information in a patient's medical record that is entered by other clinicians, rather than re-entering the information.
5. Telehealth Services
CMS will add a set of codes that describe a bundled episode of care for treatment of opioid use disorders, to the list of telehealth services covered by Medicare.
6. MIPS - 2020 performance period
45 points is the performance threshold (increased 15 points from PY 2019)
The Quality performance category is weighted at 45% (no change from PY 2019)
The Cost performance category is weighted at 15% (no change from PY 2019)
The Promoting Interoperability performance category is weighted at 25% (no change from PY 2019)
Here are the links Payment rates for major IPM codes:
Physician Fee Schedule:
https://www.asipp.org/Fee Schedules/2020PhysicianFinalRates.pdf
ASC Fee Schedule:
https://www.asipp.org/Fee Schedules/2020ASCFinalRates.pdf
HOPD Fee Schedule:
The following is important information on the newly released 2020 final payment rules. ASIPP and SIPMS will be sending comment letters to CMS. You may also send comment letters to them on these payment rules no later than 5 p.m. EST on December 2, 2019.