Good enough place as any to drop this... and the data to continues to hold that annual raw cancer cases, all dx (incl melanoma, leukemia, etc.), increases at ~20,000 pts/yr, about a 0.006% growth rate I think.
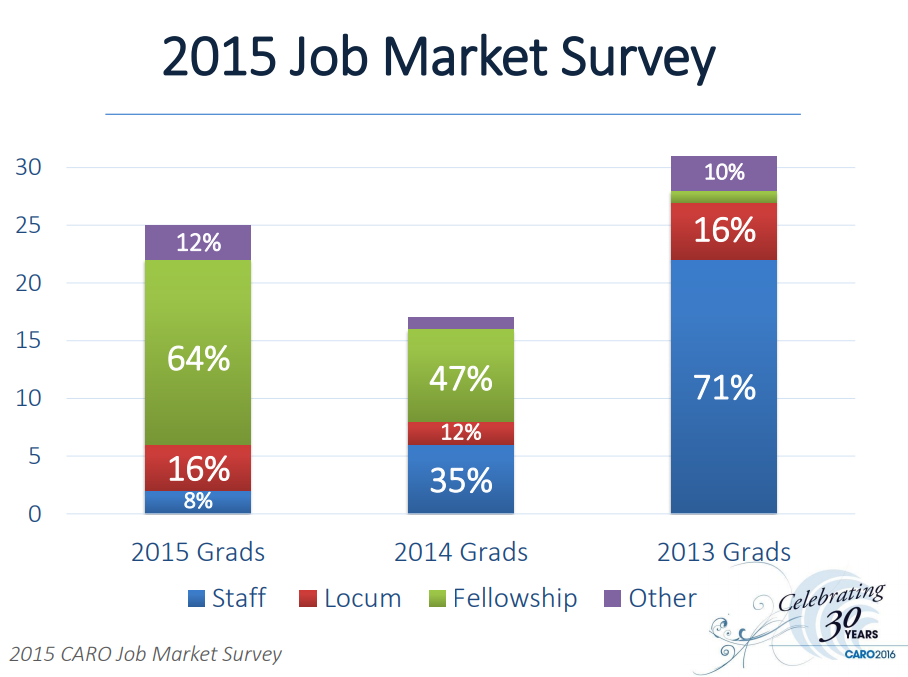
Keep in mind this would work out to about ~6000 new XRT patients/year, which works out to the concerning figure of only ~30 new patients/yr for every new resident... at current numbers. My projection seemed like it could go this low but I didn't believe it, and didn't graph it. Now I do believe it.
(Not mentioned anywhere in article: "radiotherapy.") Remarkable statements like "lung cancer death rates have dropped by 51 percent since 1990 in men, and by 26 percent since 2002 in women, with the most rapid progress in recent years" I don't think anyone could have predicted 20-30y ago.
Cancer death rate posts biggest one-year drop ever
The 2.2 percent decline in 2017 is part of a long-term decrease in mortality rates