Choosing Wisely Lemmings are just people who've never practiced enough to have a bad outcome or aren't checking to see if they've had one. I'm not saying you neglect the guidelines, but the first rule is to do no harm (by not allowing recommendations aimed at a specific clinical scenario override general common sense). I had an ED intern tell me he watched a EM podcast (that probably has extensive disclaimers at the beginning that it's not meant for clinical practice, but teaching/fostering a discussion) and that the only thing to check in new onset HTN urgency is a troponin, no CXR, BMP, EKG etc...I get it, there's no great reason to suspect pulmonary edema, AKI, ACS but if someone presented to the ED and you had resources at your disposal like a stroke, heart attack, etc. if something happens later it would be nice to have the normal EKG, CT scan, as DC instructions to control the BP and follow up with the PCP as receipts.
Presentations change. Just look at how the patient's chief complaint magically changes from tripping over the stair to pleuritic chest pain (asked in retrospect after CTA Chest showed PE).
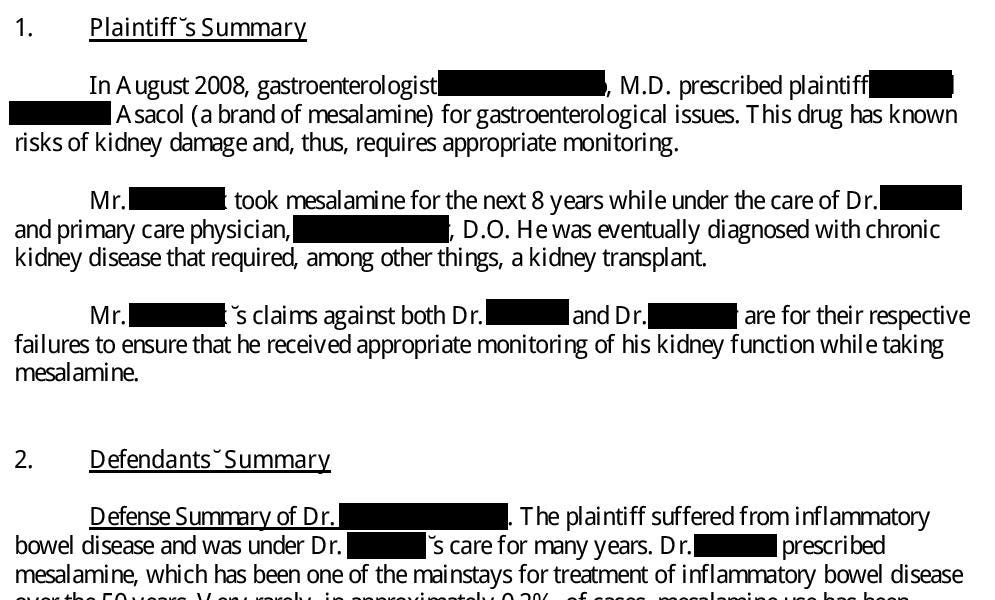
In this specific case, the GI is prescribing an NSAID that increases risk of kidney injury. GI is at fault. In the future, I'm making a streamlined system of dot-phrases, house calls, etc. for each medication I prescribe. I've seen some great practices modeled by some subspecialists I've seen in clinic. The key is to go slow, and explain every small thing that is started and each lab that is ordered and why and to document all elements for liability and billing.