In terms of things I've seen through practice questions:
1) I'd say the highest yield ECG tidbit is recognizing the absence of P-waves. Know atrial fib for sure. Sometimes they'll just show you the ECG then want you to know mural thrombus --> stroke, etc. So that's very high-yield.
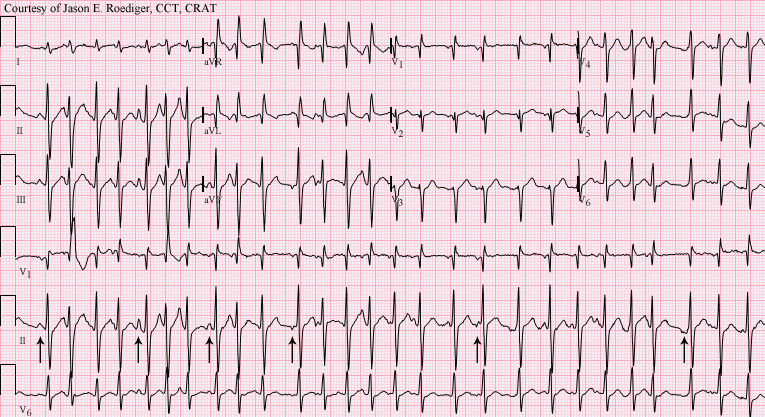
2) Know what the WPW delta-wave looks like.
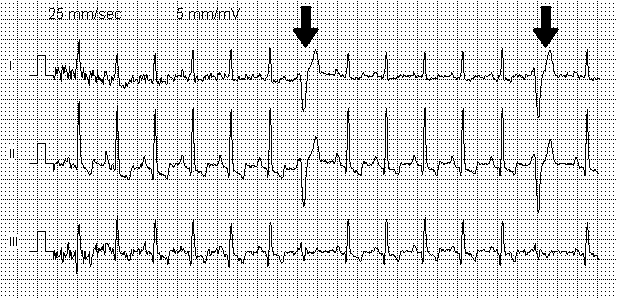
3) Be able to identify the peaked T-wave vs U-wave for hyper-/hypokalaemia. In terms of what I've seen, when they want you to identify the peaked T-wave, it's absurdly peaked, so don't flip out about it.
4) Know the spiking pattern for atrial flutter. The HR is almost always 150/min as well.
5) Simple MI (usually ST-elevation in 3 leads). It would be rare to see a posterior infarct, but be vigilant for a potential ST-depression in the anterior leads.
6) Diffuse ST-elevations +/- PR-depressions = pericarditis.
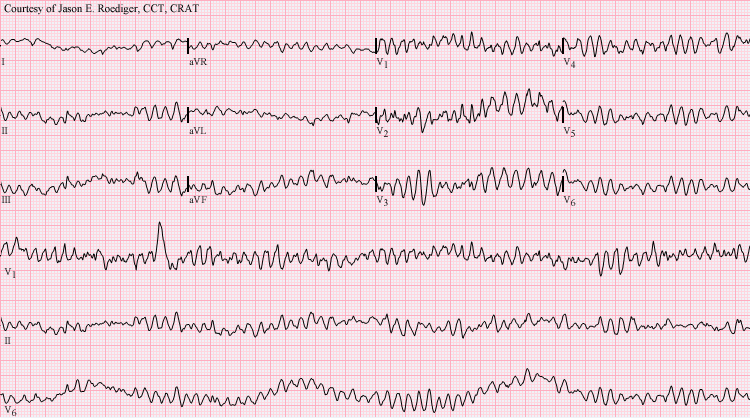
7) Sinusoidal pattern = TdP
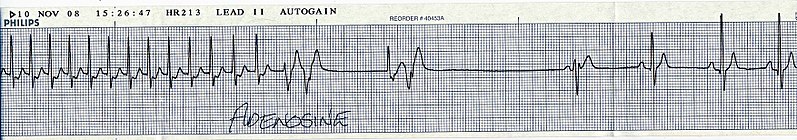
8) Wide-complex tachy = SVT with BBB, or VT. In this case, if it's one or the other, the answer is VT.
9) Mobitz I (gradually increasing PR-segments and then finally a QRS drop) + Mobitz II (random QRS drop).
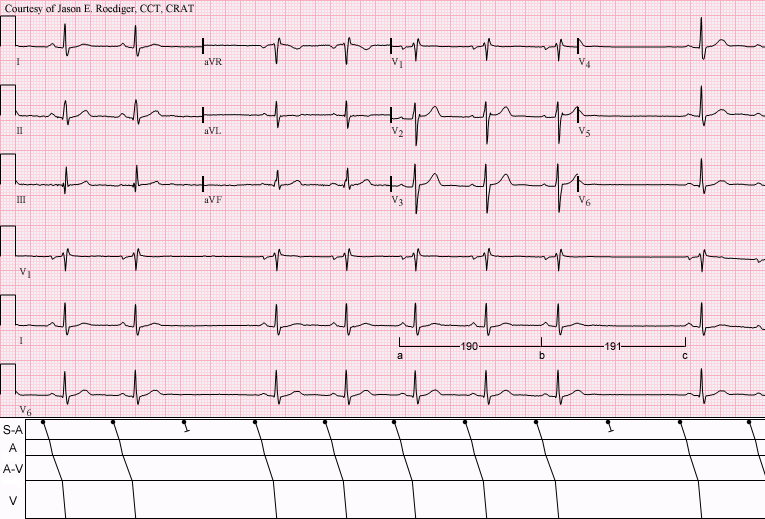
10) Complete (third-degree) heart block = QRS complexes show a HR of 30-40 and the P-waves don't have any consistent pattern relative to the QRSs.
11) And as ******ed as this sounds, know how to identify a normal ECG too. I had seen a question with a vignette of a guy with chest pain who had personal Hx of atherosclerosis and a family Hx of heart disease, but the answer was actually GERD because apparently the ECG in the question was normal. So rule of thumb: don't get tricked. I got tricked on that one needless to say. I think that may have been GT QBank.