- Joined
- Jul 14, 2007
- Messages
- 6,874
- Reaction score
- 1,357
http://economix.blogs.nytimes.com/2011/08/17/malpractice-anxiety/
I just think this is interesting how pronounced and consistent this is from when training begins.
I just think this is interesting how pronounced and consistent this is from when training begins.
Amitabh Chandra, a Harvard economist, is a leading expert on medical malpractice, and his work does not fit neatly into either the American Medical Associations camp or the trial lawyers associations camp. Sometimes it comforts one side. Sometimes, it comforts the other. I used Mr. Chandras research extensively in writing an overview of malpractice in 2009.
Now he and three other researchers have a new paper, published in The New England Journal of Medicine. Among its findings is that a large majority of malpractice claims do not lead to any payment from a doctor to a patient. Either the patient drops the case, or a court dismisses it.
In every medical specialty the researchers studied, at least three out of four claims led to no payment. In many specialties, about 9 out of 10 claims led to no payment.
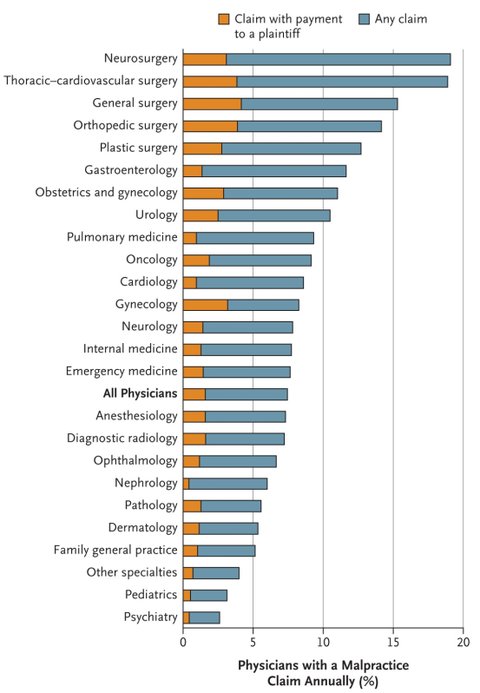
Over all, about 7 percent of doctors faced a claim in a given year, and fewer than 2 percent made any payment relating to a claim.
These patterns, the authors note, may help explain why doctors concern over malpractice suits is very high even in states that limit such suits, like Texas. As the paper notes, doctors self-reported worries about malpractice vary little across states, even though malpractice laws vary greatly. The researchers write:
Our results may speak to why physicians consistently report concern over malpractice and the intense pressure to practice defensive medicine, despite evidence that the scope of defensive medicine is modest. Although these annual rates of paid claims are low, the annual and career risks of any malpractice claim are high, suggesting that the risk of being sued alone may create a tangible fear among physicians.
The perceived threat of malpractice among physicians may boil down to three factors: the risk of a claim, the probability of a claim leading to a payment, and the size of payment. Although the frequency and average size of paid claims may not fully explain perceptions among physicians, one may speculate that the large number of claims that do not lead to payment may shape perceived malpractice risk. Physicians can insure against indemnity payments through malpractice insurance, but they cannot insure against the indirect costs of litigation, such as time, stress, added work, and reputational damage.
These findings seem consistent with earlier research suggesting that malpractice reform is nothing like a magic bullet for high medical costs. But malpractice does weigh heavily enough on doctors minds that a more efficient accountability system for doctors one in which avoidable errors were more likely to be punished and decent care was less likely to be subject to lawsuits could both improve care and have some effect on costs.
In addition to Mr. Chandra, the papers authors are Anupam B. Jena, Seth Seabury and Darius Lakdawalla.
