Thoughts on patients who are on low dose scheduled II and started on or wanting to start medical marijuana? Are you ok with patients being on both?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Medical marijuana and scheduled II
- Thread starter Bsb2015
- Start date
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
Personally I couldn't care less, but I've changed my tune legally. If you're using marijuana you get no scheduled meds from me (even though I don't care).
Thoughts on patients who are on low dose scheduled II and started on or wanting to start medical marijuana? Are you ok with patients being on both?
don't care, but the feds care
- Joined
- Feb 25, 2010
- Messages
- 4,263
- Reaction score
- 1,560
For context, I’m in a weed-illegal state. The Feds, i.e. the guys who allow me to have a DEA license at all, still consider MJ schedule I and illegal in all states. To them, it’s right there with heroin & LSD so I treat a positive as such. Don’t think for a minute that the Feds will cut you legal slack because your patients (or you or anyone else) tries to claim “weed is no big deal.” Even if you’re right, the Fed don’t agree, so it doesn’t matter. If they ever do agree, I’ll see proof of that when they legalize Federally. Until then, “Sorry, it sucks but, Feds’ rules not mine. Sorry.” Bye.
Plus, I think it’s bulls**t that people claim they smoke cannabis for their pain, but then they all still want opiates. Argues to me, that medical cannabis (for pain, at least) is likely a fraud. Plus, the Feds will be glad to make an example of you by claiming you knew or should have known they sold your pills to buy pot, which again, according to all their laws is 100% illegal in a 50 states.
In 2019 we should be looking for reasons to discontinue opiates, not looking for reasons to rationalize continuing them. When you find such a reason, act on it.
Plus, I think it’s bulls**t that people claim they smoke cannabis for their pain, but then they all still want opiates. Argues to me, that medical cannabis (for pain, at least) is likely a fraud. Plus, the Feds will be glad to make an example of you by claiming you knew or should have known they sold your pills to buy pot, which again, according to all their laws is 100% illegal in a 50 states.
In 2019 we should be looking for reasons to discontinue opiates, not looking for reasons to rationalize continuing them. When you find such a reason, act on it.
Last edited:
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
if you have THC and opioids in UDS you are not in compliance and may be prosecuted.
This is my bottom line, and the reason I DC all scheduled meds on any pt with THC in the UDS. I told a guy today I don't care if he uses CBD oil but a dirty UDS is a dirty UDS and he's a work comp guy I'm trying to wean off Percocet. If he pops for THC it is DC with no wean...baclofen, clonidine, Zofran...
To be legal, CBD oil must be less than 0.3% THC but you can still pop for it, and I have a fear of dudes using CBD just so they can blame their failed urine on it when they are actually smoking weed.
- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
I don't allow both, but I'll give them a warning and a chance to stop before discharge off opiates. Other drugs is one and done from office.
I don't get where people think that marijuana is "safe". There is a ton of evidence that it causes real harm. Here's my template and the packet I give patients.
Patient has been identified as a user of marijuana products. While legal at the state level under certain circumstances, marijuana is still considered by the federal government to be a Schedule-1 controlled substance. Schedule-1 substances are defined as drugs with no accepted medical use and high potential for abuse, potentially leading to severe psychological or physical dependence. Marijuana use has also been associated with impaired body movement, difficulty thinking and problem-solving, impaired memory, anxiety, depression, hallucinations, early-onset psychosis, paranoia, poor school performance, and decreased IQ. In addition, users of marijuana have been shown to have lower life satisfaction, poorer physical and mental health, less academic and career success, and more job absences, accidents, and injuries. In addition, people who use marijuana have been shown to be more likely to use prescription drugs for both medical and nonmedical purposes. I recommend the patient stop using marijuana products.
Drug Fact sheet from the NIH has been given to the patient regarding marijuana.
Marijuana
If they insist on marijuana use, I don't stop treating them (I'm in a recreational "legal" state), just no opiates from me.
I don't get where people think that marijuana is "safe". There is a ton of evidence that it causes real harm. Here's my template and the packet I give patients.
Patient has been identified as a user of marijuana products. While legal at the state level under certain circumstances, marijuana is still considered by the federal government to be a Schedule-1 controlled substance. Schedule-1 substances are defined as drugs with no accepted medical use and high potential for abuse, potentially leading to severe psychological or physical dependence. Marijuana use has also been associated with impaired body movement, difficulty thinking and problem-solving, impaired memory, anxiety, depression, hallucinations, early-onset psychosis, paranoia, poor school performance, and decreased IQ. In addition, users of marijuana have been shown to have lower life satisfaction, poorer physical and mental health, less academic and career success, and more job absences, accidents, and injuries. In addition, people who use marijuana have been shown to be more likely to use prescription drugs for both medical and nonmedical purposes. I recommend the patient stop using marijuana products.
Drug Fact sheet from the NIH has been given to the patient regarding marijuana.
Marijuana
If they insist on marijuana use, I don't stop treating them (I'm in a recreational "legal" state), just no opiates from me.
Attachments
- Joined
- Feb 25, 2010
- Messages
- 4,263
- Reaction score
- 1,560
To be legal, CBD oil must be less than 0.3% THC but you can still pop for it, and I have a fear of dudes using CBD just so they can blame their failed urine on it when they are actually smoking weed.
Exactly. And the DEAs response to those blowing off a THC + UDS based on CBD oil is going to be, "Sorry. You ignored THC. THC is schedule I and illegal per Federal law. Period."
- Joined
- Jun 28, 2006
- Messages
- 202
- Reaction score
- 22
for those of you who manage opioid dependency, do you apply the same rules with marijuana and Suboxone?
- Joined
- Nov 21, 1998
- Messages
- 12,563
- Reaction score
- 6,954
for those of you who manage opioid dependency, do you apply the same rules with marijuana and Suboxone?
Suboxone is an opioid and a scheduled drug too.
- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
for those of you who manage opioid dependency, do you apply the same rules with marijuana and Suboxone?
I don't manage opiate dependency/abuse, however from what I understand, there is more tolerance to "slip ups" in that patient population since the goal is to control their addiction, not treat pain.
- Joined
- May 28, 2003
- Messages
- 1,070
- Reaction score
- 37
Ditto. Except for Lyrica.Personally I couldn't care less, but I've changed my tune legally. If you're using marijuana you get no scheduled meds from me (even though I don't care).
- Joined
- May 28, 2003
- Messages
- 1,070
- Reaction score
- 37
Yesfor those of you who manage opioid dependency, do you apply the same rules with marijuana and Suboxone?
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953

Cannabis users may need more anesthesia for surgery
People who regularly use cannabis may need more than twice the usual dose of anesthesia for surgery, a U.S. study suggests.
- Joined
- May 30, 2005
- Messages
- 21,244
- Reaction score
- 12,358

Cannabis users may need more anesthesia for surgery
People who regularly use cannabis may need more than twice the usual dose of anesthesia for surgery, a U.S. study suggests.www.reuters.com
Fun study. But beyond useless. They had 25 self reported marijuana users out of 250 patients undergoing colonoscopy. Self reported use. Not tested for. And percent additional meds used was less than 20%. Lots of potential confounders. But fun to postulate. Not worthy of publication in a peer reviewed journal.
- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
As an anesthesiologist, this 100% matches my experience.
Cannabis users may need more anesthesia for surgery
People who regularly use cannabis may need more than twice the usual dose of anesthesia for surgery, a U.S. study suggests.www.reuters.com
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
useless maybe, but it is more evidence of potential ill effects of marijuana than positive evidence showing benefit of marijuana for chronic pain.
- Joined
- Feb 11, 2019
- Messages
- 36
- Reaction score
- 40
In my personal world, I dont care. In my professional/work arena, I say NO to mj. As long as its federally illegal i just cant deal with it. You never know when the tide will turn against medical marijuana just like it did with opioids...All it will take is some poorly written, overapplied set of guidelines...(sound familiar?).
As far as I know, cannabis is legalized in Canada and is often used in medicine. I believe that this is a big development in this area and many positive reviews can be read from patients about cannabis treatment. Fortunately, there are many services in Canada that allow you to buy cheap cannabis shatter and use it for your own purposes. Anyone can use cannabis to relax, improve their sleep and their physical condition. I hope that in the future in many countries the legalization of cannabis will be successful and medicine will approve of its use.
Last edited:
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
have to be careful about $ome of tho$e review$ and whether they are being generated by tho$e in pain or otherwi$e.
id like to see data about how many people who get put on medical marijuana are able to come off of opioid therapy.
id like to see data about how many people who get put on medical marijuana are able to come off of opioid therapy.
- Joined
- May 30, 2005
- Messages
- 21,244
- Reaction score
- 12,358
have to be careful about $ome of tho$e review$ and whether they are being generated by tho$e in pain or otherwi$e.
id like to see data about how many people who get put on medical marijuana are able to come off of opioid therapy.
marijuana only works when I take it with the percs.
- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
This is the best study I've been able to find. Most of the "studies" out there are complete crap.have to be careful about $ome of tho$e review$ and whether they are being generated by tho$e in pain or otherwi$e.
id like to see data about how many people who get put on medical marijuana are able to come off of opioid therapy.
Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings from a 4-year prospective cohort study
Summary
Background
Interest in the use of cannabis and cannabinoids to treat chronic non-cancer pain is increasing, because of their potential to reduce opioid dose requirements. We aimed to investigate cannabis use in people living with chronic non-cancer pain who had been prescribed opioids, including their reasons for use and perceived effectiveness of cannabis; associations between amount of cannabis use and pain, mental health, and opioid use; the effect of cannabis use on pain severity and interference over time; and potential opioid-sparing effects of cannabis.Methods
The Pain and Opioids IN Treatment study is a prospective, national, observational cohort of people with chronic non-cancer pain prescribed opioids. Participants were recruited through community pharmacies across Australia, completed baseline interviews, and were followed up with phone interviews or self-complete questionnaires yearly for 4 years. Recruitment took place from August 13, 2012, to April 8, 2014. Participants were asked about lifetime and past year chronic pain conditions, duration of chronic non-cancer pain, pain self-efficacy, whether pain was neuropathic, lifetime and past 12-month cannabis use, number of days cannabis was used in the past month, and current depression and generalised anxiety disorder. We also estimated daily oral morphine equivalent doses of opioids. We used logistic regression to investigate cross-sectional associations with frequency of cannabis use, and lagged mixed-effects models to examine temporal associations between cannabis use and outcomes.Findings
1514 participants completed the baseline interview and were included in the study from Aug 20, 2012, to April 14, 2014. Cannabis use was common, and by 4-year follow-up, 295 (24%) participants had used cannabis for pain. Interest in using cannabis for pain increased from 364 (33%) participants (at baseline) to 723 (60%) participants (at 4 years). At 4-year follow-up, compared with people with no cannabis use, we found that participants who used cannabis had a greater pain severity score (risk ratio 1·14, 95% CI 1·01–1·29, for less frequent cannabis use; and 1·17, 1·03–1·32, for daily or near-daily cannabis use), greater pain interference score (1·21, 1·09–1·35; and 1·14, 1·03–1·26), lower pain self-efficacy scores (0·97, 0·96–1·00; and 0·98, 0·96–1·00), and greater generalised anxiety disorder severity scores (1·07, 1·03–1·12; and 1·10, 1·06–1·15). We found no evidence of a temporal relationship between cannabis use and pain severity or pain interference, and no evidence that cannabis use reduced prescribed opioid use or increased rates of opioid discontinuation.Interpretation
Cannabis use was common in people with chronic non-cancer pain who had been prescribed opioids, but we found no evidence that cannabis use improved patient outcomes. People who used cannabis had greater pain and lower self-efficacy in managing pain, and there was no evidence that cannabis use reduced pain severity or interference or exerted an opioid-sparing effect. As cannabis use for medicinal purposes increases globally, it is important that large well designed clinical trials, which include people with complex comorbidities, are conducted to determine the efficacy of cannabis for chronic non-cancer pain.- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
- Joined
- Nov 21, 1998
- Messages
- 12,563
- Reaction score
- 6,954
Here's the article:
It's not a RCT.
No Xannie bars?....you worst doc evermarijuana only works when I take it with the percs.
- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
Yep, best I can find. You know of a good RCT? Post it here if you do.It's not a RCT.
- Joined
- Nov 21, 1998
- Messages
- 12,563
- Reaction score
- 6,954
Randomized Controlled TrialYep, best I can find. You know of a good RCT? Post it here if you do.
Eur J Neurol
2007 Mar;14(3):290-6.
doi: 10.1111/j.1468-1331.2006.01639.x.
Randomized controlled trial of cannabis-based medicine in spasticity caused by multiple sclerosis
C Collin 1, P Davies, I K Mutiboko, S Ratcliffe, Sativex Spasticity in MS Study GroupAffiliations expand
- PMID: 17355549
- DOI: 10.1111/j.1468-1331.2006.01639.x
Abstract
Symptoms relating to spasticity are common in multiple sclerosis (MS) and can be difficult to treat. We have investigated the efficacy, safety and tolerability of a standardized oromucosal whole plant cannabis-based medicine (CBM) containing delta-9 tetrahydrocannabinol (THC) and cannabidiol (CBD), upon spasticity in MS. A total of 189 subjects with definite MS and spasticity were randomized to receive daily doses of active preparation (n = 124) or placebo (n = 65) in a double blind study over 6 weeks. The primary endpoint was the change in a daily subject-recorded Numerical Rating Scale of spasticity. Secondary endpoints included a measure of spasticity (Ashworth Score) and a subjective measure of spasm. The primary efficacy analysis on the intention to treat (ITT) population (n = 184) showed the active preparation to be significantly superior (P = 0.048). Secondary efficacy measures were all in favour of active preparation but did not achieve statistical significance. The responder analysis favoured active preparation, 40% of subjects achieved >30% benefit (P = 0.014). Eight withdrawals were attributed to adverse events (AEs); six were on active preparation and two on placebo. We conclude that this CBM may represent a useful new agent for treatment of the symptomatic relief of spasticity in MS.- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
interesting old study.
not pertinent to the topic of discussion.
to reiterate - what is the data to suggest that medical marijuana reduces opioid use?
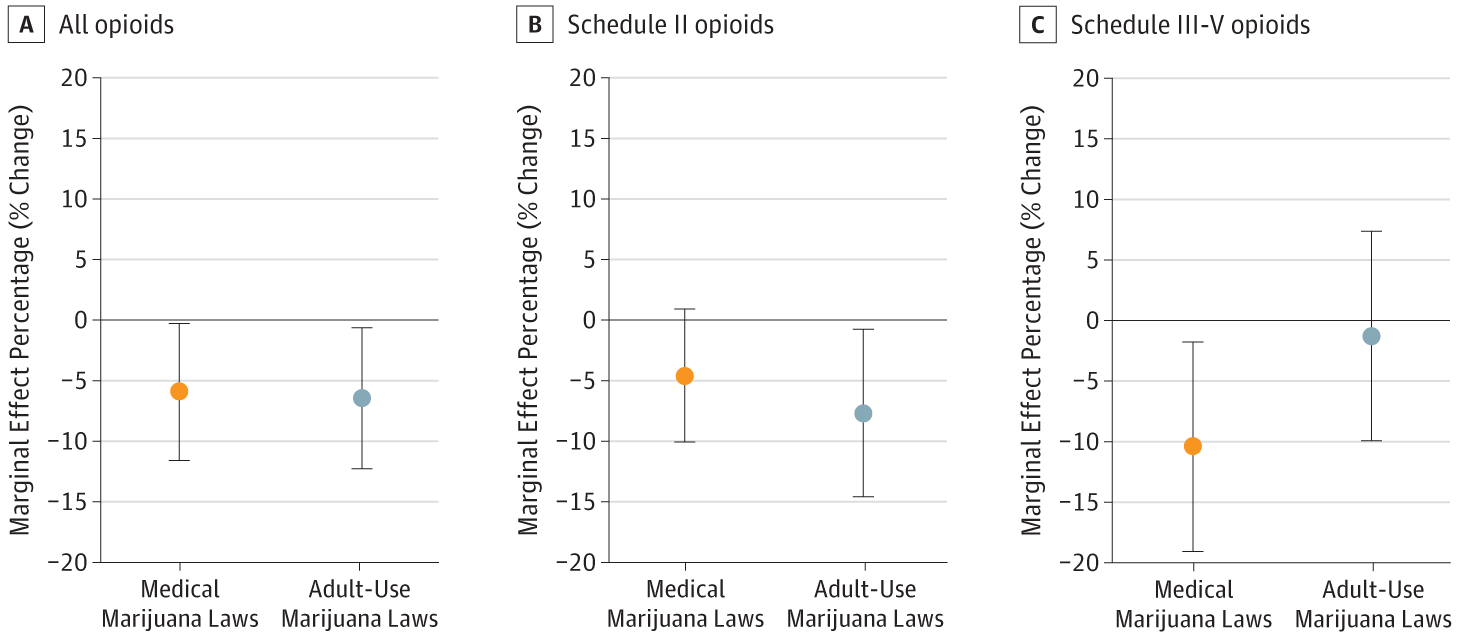
there is some population data (not individualized) to suggest that legalizing medical marijuana does reduce opioid prescribing... but I am not clear if this is due to changes in prescriber behavior or pain management, because some of the studies suggest that legal marijuana does not help that much with pain....
 jamanetwork.com
jamanetwork.com
now here is confounding information:
 www.drugabuse.gov
www.drugabuse.gov
not pertinent to the topic of discussion.
to reiterate - what is the data to suggest that medical marijuana reduces opioid use?
there is some population data (not individualized) to suggest that legalizing medical marijuana does reduce opioid prescribing... but I am not clear if this is due to changes in prescriber behavior or pain management, because some of the studies suggest that legal marijuana does not help that much with pain....
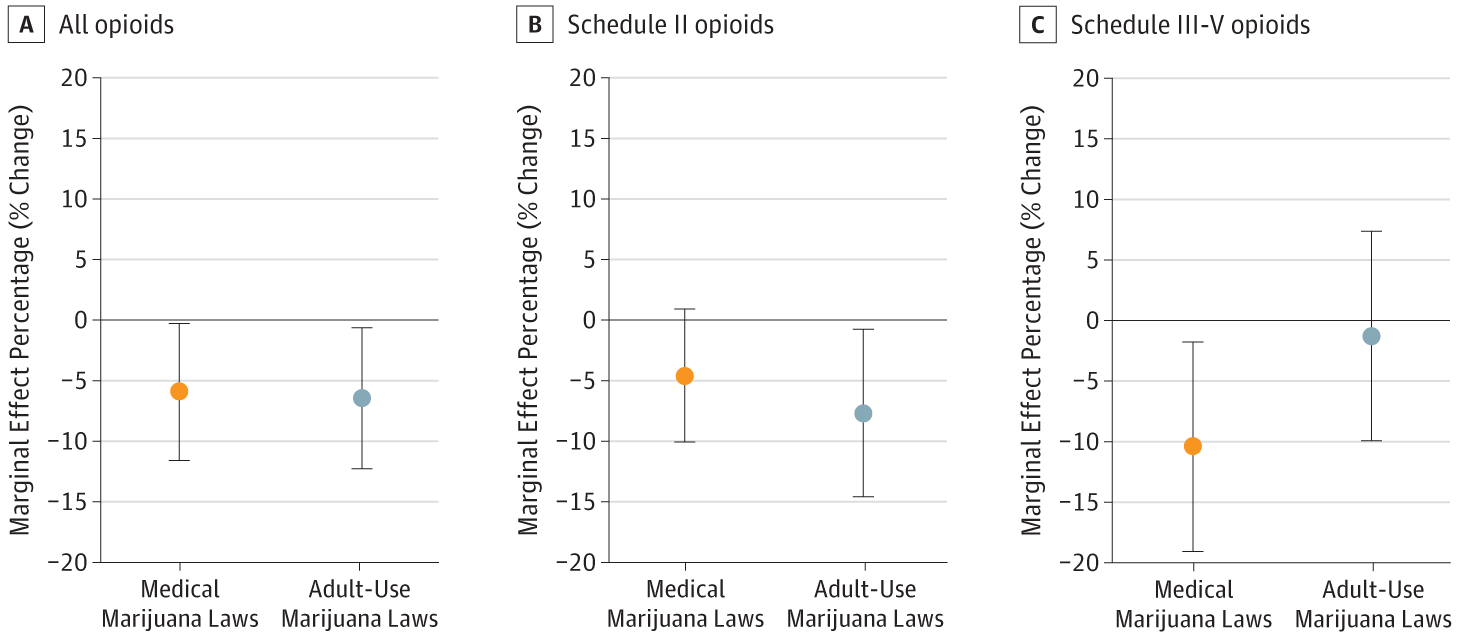
Medical and Adult-Use Marijuana Laws and Opioid Prescribing for Medicaid Enrollees
This population-based, cross-sectional study examines the association of state implementation of medical and adult-use marijuana laws with opioid prescribing rates and spending among Medicaid enrollees.
now here is confounding information:
Medical Marijuana Laws and Opioid Overdose Rates | NIDA Archives
A new study underscores the need for additional research on the effect of medical marijuana laws on opioid overdose deaths and cautions against drawing a causal connection between the two.
which brings me back to above point - was opioid prescribing and opioid related harm (ie OD) related to changes in physician behavior ie decreased prescribing rather than marijuana itself?In particular, a NIDA-funded study published in 2014 found that from 1999 to 2010, states with medical cannabis laws experienced slower rates of increase in opioid analgesic overdose death rates compared to states without such laws. A 2019 analysis, also funded by NIDA, re-examined this relationship using data through 2017. Similar to the findings reported previously, this research team found that opioid overdose mortality rates between 1999-2010 in states allowing medical marijuana use were 21% lower than expected. When the analysis was extended through 2017, however, they found that the trend reversed, such that states with medical cannabis laws experienced an overdose death rate 22.7% higher than expected. The investigators uncovered no evidence that either broader cannabis laws (those allowing recreational use) or more restrictive laws (those only permitting the use of marijuana with low tetrahydrocannabinol concentrations) were associated with changes in opioid overdose mortality rates.
- Joined
- Nov 21, 1998
- Messages
- 12,563
- Reaction score
- 6,954
interesting old study.
not pertinent to the topic of discussion.
to reiterate - what is the data to suggest that medical marijuana reduces opioid use?
there is some population data (not individualized) to suggest that legalizing medical marijuana does reduce opioid prescribing... but I am not clear if this is due to changes in prescriber behavior or pain management, because some of the studies suggest that legal marijuana does not help that much with pain....
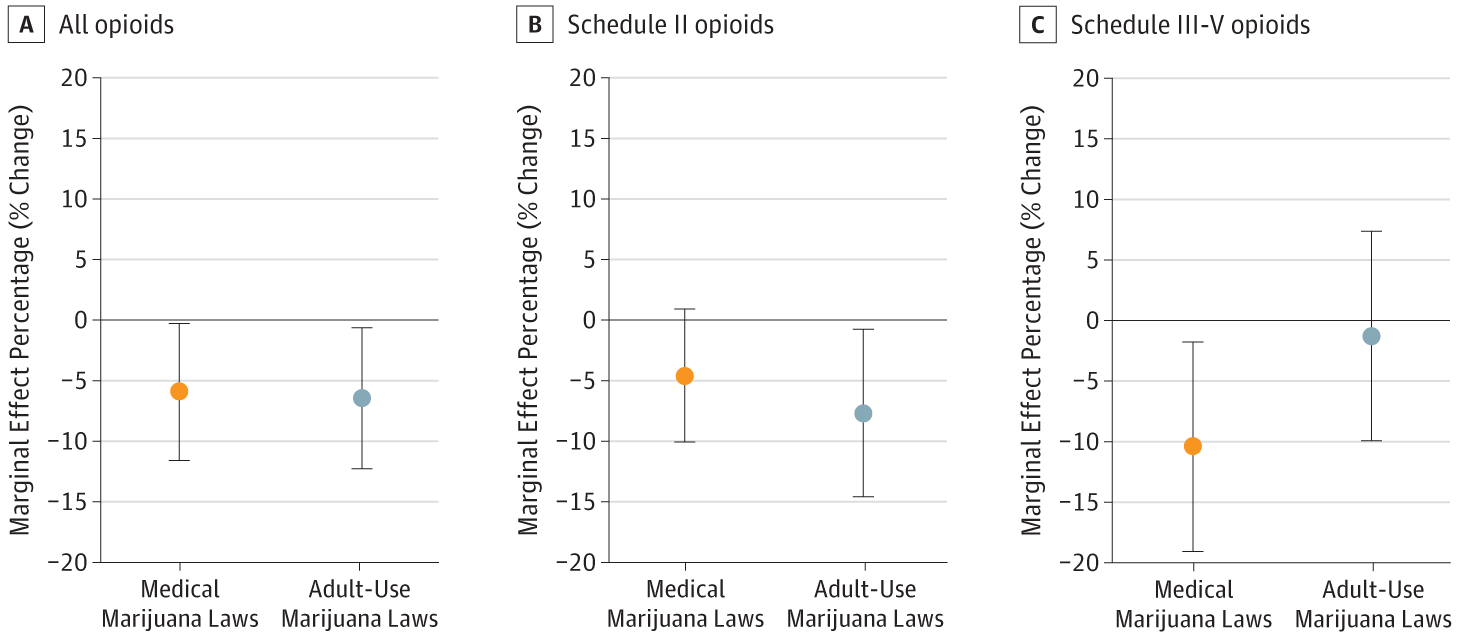
Medical and Adult-Use Marijuana Laws and Opioid Prescribing for Medicaid Enrollees
This population-based, cross-sectional study examines the association of state implementation of medical and adult-use marijuana laws with opioid prescribing rates and spending among Medicaid enrollees.jamanetwork.com
now here is confounding information:
Medical Marijuana Laws and Opioid Overdose Rates | NIDA Archives
A new study underscores the need for additional research on the effect of medical marijuana laws on opioid overdose deaths and cautions against drawing a causal connection between the two.www.drugabuse.gov
which brings me back to above point - was opioid prescribing and opioid related harm (ie OD) related to changes in physician behavior ie decreased prescribing rather than marijuana itself?
The old studies stand the test of time.
- Joined
- Dec 12, 2006
- Messages
- 2,981
- Reaction score
- 3,483
Especially studies with an N of 189 for spasticityThe old studies stand the test of time.
D
deleted875186
Interesting study, I agree as an anesthesiologist this 100% is true.Fun study. But beyond useless. They had 25 self reported marijuana users out of 250 patients undergoing colonoscopy. Self reported use. Not tested for. And percent additional meds used was less than 20%. Lots of potential confounders. But fun to postulate. Not worthy of publication in a peer reviewed journal.
self reporting marijuana use - probably more reliable than testing for it in this type of study, we are looking for chronic use rather than short term use.
colonoscopy - these type of procedures, MAC, are the only way to see “how much anesthesia” a patient requires. A standard GA with muscle relaxant is not useful, patient will be paralyzed and just lighter plane of anesthesia, harder to tell how much prop they require.
I personally like the study. This type of study will never be perfect. Certainly can never have a RCT on it.
D
deleted314957
If the Feds would remove it from schedule 1 , the academic and pharmaceutical industry could much more easily do solid research as regards cannabinoids.
Similar threads
- Replies
- 3
- Views
- 611
