- Joined
- May 7, 2008
- Messages
- 479
- Reaction score
- 465
I was curious if anyone had any journal articles from the past relating to anesthesia that they felt were must reads for people in the field.
Not specific to anesthesia but it would certainly affect your practice. If you only read one article any given year, read the Surviving Sepsis guidelines. As for others, one can easily look up past landmark studies. Most relate in some way to our specialty.
I was curious if anyone had any journal articles from the past relating to anesthesia that they felt were must reads for people in the field.
YES!!
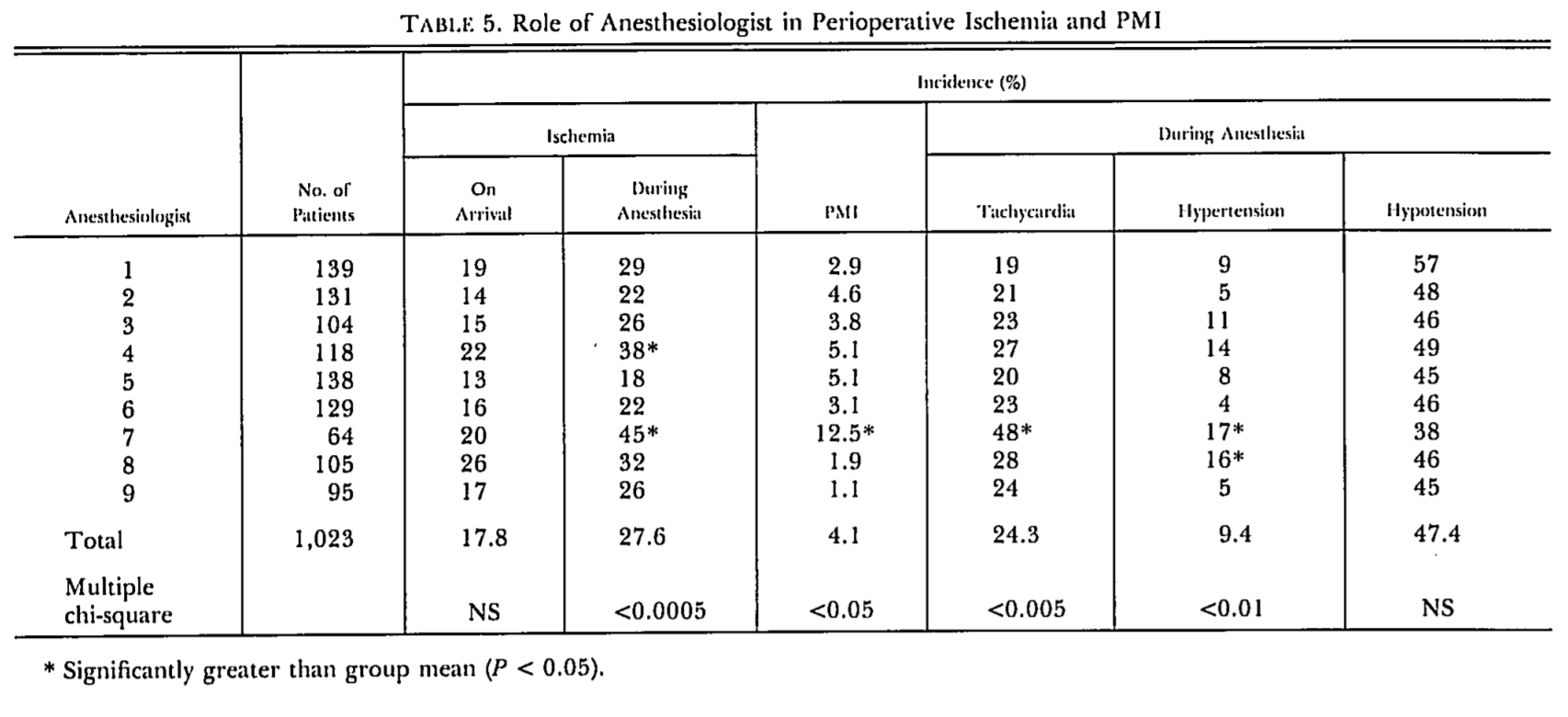
This is one that every resident should read, if nothing else to learn the legend of 'anesthesiologist #7': Does perioperative myocardial ischemia lead to postoperative myocardial infarction? - PubMed - NCBI
Not only is Surviving Sepsis a terrible document based almost entirely off Manny Rivers' terribly flawed trial, but I would also argue that it's not very useful from an anesthesia standpoint. The ED/floor/surgical team will almost certainly have already drowned the patient in fluids and chosen some cocktail of broad spectrum antibiotics. As anesthesiologists, we're in a prime position to watch the patient minute by minute and figure out how their hemodynamics and physiology react to different strategies as opposed to using an assembly line approach.YES!!
I didn't read the entire 160+ pages of surviving sepsis guideline. But i did read a lot of it on one of my researches. A lot of the "evidence" is based on very ****ty studies. It's like if you wrap **** up into many layers, it stops smelling and people accept it.
Also it's not a guideline in a lot of academia. At my mid tier residency, the surviving sepsis guideline is more like dogma. The way it almost prohibitively favors norepi over all other vaso active agents is idiotic. I hate this document slightly less than Mao and Al Qaeda. You are an anesthesiologist. The problems are distributive shock and bacteremia. You don't need a dogmatic document to tell you how to treat those problems....
/end rant. I signed the petition.
 ”
”I wonder what happened to #7. Looks like they fired him halfway through.The legend ...
YES!!
I didn't read the entire 160+ pages of surviving sepsis guideline. But i did read a lot of it on one of my researches. A lot of the "evidence" is based on very ****ty studies. It's like if you wrap **** up with many layers, it stops smelling eventually and people accept it.
Also it's not a guideline in a lot of academia. At my mid tier residency, the surviving sepsis guideline is more like dogma. The way it almost prohibitively favors norepi over all other vaso active agents is idiotic. I hate this document slightly less than Mao and Al Qaeda. You are an anesthesiologist. The problems are distributive shock and bacteremia. You don't need a dogmatic document to tell you how to treat those problems....
/end rant. I signed the petition.
Someone once told me they did a study on septic pts on different pressers and measured gut mucosa blood flow with some type of say probe and found norepi to give the best perfusion. I’ve never been able to find it though, anyone know of something like this?Which pressor would you prefer in sepsis? Sometimes I think the afib or very tachy patients would benefit from phenylephrine gtt but then people look at me like I'm crazy...
Someone once told me they did a study on septic pts on different pressers and measured gut mucosa blood flow with some type of say probe and found norepi to give the best perfusion. I’ve never been able to find it though, anyone know of something like this?
Which pressor would you prefer in sepsis? Sometimes I think the afib or very tachy patients would benefit from phenylephrine gtt but then people look at me like I'm crazy...
That's exactly my first go to drug in tachycardia, unless the patient has a decreased EF. I watch the BP closely. If I don't see it going up as the HR is coming down, my next go-to drug is norepi.Which pressor would you prefer in sepsis? Sometimes I think the afib or very tachy patients would benefit from phenylephrine gtt but then people look at me like I'm crazy...
... One constant in medical history has been the number of beliefs and certainties that end up being false.
What do you mean by under-resuscitated?Not to hijack a thread, but I know that sepsis guidelines changed during my residency and haven't gotten around to reading them. Anecdotally, I notice more and more patients in septic shock being treated with norepinephrine infusions titrated to NIBP pressures and who always appear to be under-resuscitated. These patients are just setup to crash in the OR. Is there something in the new guidelines causing this?
It begins in middle school science fairs where lots of data is made up BS. As a species we are not suited to perform good science which is often laborious and tedious and unrewarding.
Imho the problem is that MDs are too emotionally and financially invested to apply the 13th law of the House of God.That, plus the fact that we are simply unable to grasp the value of studies that show a non-effect of an intervention. Drug and device development is so costly that there will never be a paradigm where researchers who find a drug or device ineffective in a large phase 3 trial will be rewarded for the service they performed.
What do you mean by under-resuscitated?
If you mean that they are not pumped full of saltwater anymore, that's good. Btw, any patient with sepsis (hence decreased SVR and possibly distributive shock) will have a risk of crashing after more vasodilators (e.g. general anesthesia) are applied. The solution is giving more vasoconstrictors first (e.g. boluses of norepi before induction etc.), not fluids (unless you can prove that the patient is both hypovolemic and fluid-responsive, which is complicated).
I haven't read this yet (it's on my list), but, based on its authors, I would be surprised if it's not a great paper, even for anesthesiologists: Intravenous fluid therapy in critically ill adults | Nature Reviews Nephrology (it takes OpenAthens, which many of you should have at work).
The main problem with anesthesiologists and intensivists nowadays is not that we haven't read the "great" papers; it's that we don't know modern physiology and pathophysiology because we don't keep current with the literature, and especially the great blogs and minds of our fields. It requires time and dedication, but it's always heartbreaking to see an anesthesiologist or intensivist who still treats her patients as if it's still 2008. E.g. one who recommends the Surviving Sepsis Campaign guidelines or the famously unethical (and repeatedly disproven) Emanuel Rivers study.
I personally find that being up-to-date with the critical care literature also makes me a better anesthesiologist for my sicker patients. Good starting points for that would be www.emcrit.org, www.lifeinthefastlane.com and http://maryland.ccproject.com. Don't hesitate to learn resus or airway management from EM docs/blogs; they deal with some of the same problems as anesthesiologists and intensivists.
I strongly suggest spending time on review articles, even on blogs, versus individual papers. Breadth and perspective should come before depth, or you'll end up wasting time on stuff that has been proven irrelevant. Read the papers whose abstracts or summaries (on good blogs) suggest that they apply to your patient population, not just the "great" papers, and take everything with a grain of salt. E.g., the famous ARDSNet paper only proved that 6 ml/kg is better than 12 ml/kg of tidal volume. Who the heck uses 12 ml/kg? Know the big picture of as many good papers as possible, not the details of a few "great" ones. Breadth first.
Also, remember @BLADEMDA. Such an inspiration for anybody who wants to become more knowledgeable about anesthesia. Just look up his posts, many of which point to relevant papers.
I have every intention to start reading this stuff now that I finished residency and have a bit more free time
To illustrate what I mean by under-resuscitated this is the most recent case I had:
60ish y/o male with PMH of HTN and HLD only presented to OSH with C.diff and treated OP. Patient developed toxic mega colon and was transferred to our hospital. He spent a day in the ICU to be "resuscitated". He receiving 7 or 8 liters of crystalloid in total during that time and was started on antibiotics. That seems reasonable to me. They started norepinephrine a few liters in and titrated it to a cuff pressure (drives me nuts that this is so so commonplace for surgical patients). Clearly the inciting pathology was worsening as the patient became increasingly acidotic (lactate was above 4 when he came to the OR) and went into AKI. Instead of intubating the patient early, adding pressors, and potentially starting HD, he was started on a bicarb drip and maxed on a single pressor. When I saw the guy, he was on the verge of also going into respiratory failure. Preinduction arterial line and gas right after intubation showed a pH of 7.22. I treated him as a cardiac-RSI induction and he still predictably tanked right after.
This pseudo-resuscitated surgical patient seems almost commonplace at both my training program and new hospital. Obviously he wasn't getting better w/o surgery but there's a lot that could've been done to prepare him better for surgery. Where I trained, it was typical to get patients in septic shock d/t gangrene in similar conditions. Just wondering if something in there literature has lead to this.
I have every intention to start reading this stuff now that I finished residency and have a bit more free time
To illustrate what I mean by under-resuscitated this is the most recent case I had:
60ish y/o male with PMH of HTN and HLD only presented to OSH with C.diff and treated OP. Patient developed toxic mega colon and was transferred to our hospital. He spent a day in the ICU to be "resuscitated". He receiving 7 or 8 liters of crystalloid in total during that time and was started on antibiotics. That seems reasonable to me. They started norepinephrine a few liters in and titrated it to a cuff pressure (drives me nuts that this is so so commonplace for surgical patients). Clearly the inciting pathology was worsening as the patient became increasingly acidotic (lactate was above 4 when he came to the OR) and went into AKI. Instead of intubating the patient early, adding pressors, and potentially starting HD, he was started on a bicarb drip and maxed on a single pressor. When I saw the guy, he was on the verge of also going into respiratory failure. Preinduction arterial line and gas right after intubation showed a pH of 7.22. I treated him as a cardiac-RSI induction and he still predictably tanked right after.
This pseudo-resuscitated surgical patient seems almost commonplace at both my training program and new hospital. Obviously he wasn't getting better w/o surgery but there's a lot that could've been done to prepare him better for surgery. Where I trained, it was typical to get patients in septic shock d/t gangrene in similar conditions. Just wondering if something in there literature has lead to this.
Now if I say that the 7-8L of crystalloid in a day may have caused his AKI... you'll say I am nuts. But it's very possible (hypotension combined with renal venous congestion/intra-abdominal hypertension, especially in the context of an already distended bowel), unless there was a lot of fluid loss through diarrhea (which may also explain the bicarb drip - since the patient's acidosis would have been also due to loss of bicarbonate).I have every intention to start reading this stuff now that I finished residency and have a bit more free time
To illustrate what I mean by under-resuscitated this is the most recent case I had:
60ish y/o male with PMH of HTN and HLD only presented to OSH with C.diff and treated OP. Patient developed toxic mega colon and was transferred to our hospital. He spent a day in the ICU to be "resuscitated". He receiving 7 or 8 liters of crystalloid in total during that time and was started on antibiotics. That seems reasonable to me. They started norepinephrine a few liters in and titrated it to a cuff pressure (drives me nuts that this is so so commonplace for surgical patients). Clearly the inciting pathology was worsening as the patient became increasingly acidotic (lactate was above 4 when he came to the OR) and went into AKI. Instead of intubating the patient early, adding pressors, and potentially starting HD, he was started on a bicarb drip and maxed on a single pressor. When I saw the guy, he was on the verge of also going into respiratory failure. Preinduction arterial line and gas right after intubation showed a pH of 7.22. I treated him as a cardiac-RSI induction and he still predictably tanked right after.
This pseudo-resuscitated surgical patient seems almost commonplace at both my training program and new hospital. Obviously he wasn't getting better w/o surgery but there's a lot that could've been done to prepare him better for surgery. Where I trained, it was typical to get patients in septic shock d/t gangrene in similar conditions. Just wondering if something in there literature has lead to this.
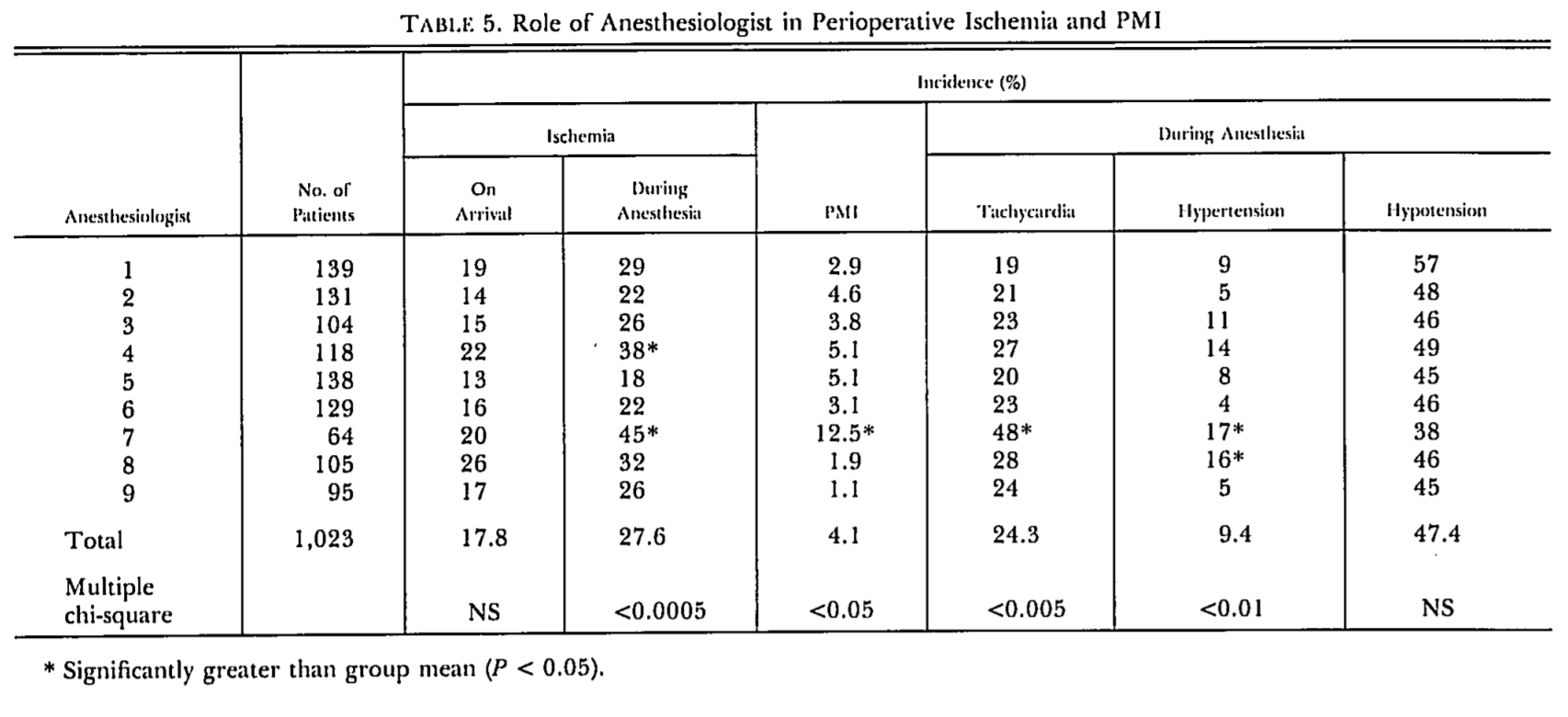
All this sepsis talk reminds me of this case: Pt comes back into the OR tachy to 130s with mental status changes for re op to drain another abdominal abscess. She is on one drip: Cardizem. I turned it off and got the case started then started looking though the notes to find out why she was on cardizem. This was the cardiologist last note before pt went to the OR....
View attachment 240348
All this sepsis talk reminds me of this case: Pt comes back into the OR tachy to 130s with mental status changes for re op to drain another abdominal abscess. She is on one drip: Cardizem. I turned it off and got the case started then started looking though the notes to find out why she was on cardizem. This was the cardiologist last note before pt went to the OR....
He didn't post anything different than the case vignettes we all post here all the time. Nothing there that's even close to being identifying information. We don't even know what country he's in.Dunno about where you work, but if I took a picture of a patient's chart and posted it on an internet forum I just might get fired.
He didn't post anything different than the case vignettes we all post here all the time. Nothing there that's even close to being identifying information. We don't even know what country he's in.
These are two MUST READS!
Let me know what you think if you haven't read them before.
