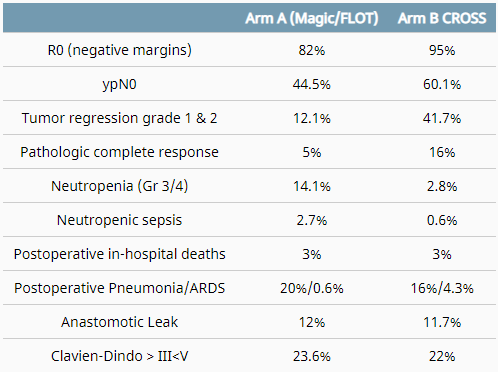
I'm at a major academic center and the other day it was suggested that we should start considering neoadjuvant chemo alone for distal esophageal cancers based on this abstract at ASCO. Every single reported metric in the table below was superior for CROSS and yet the conclusion was "the data strongly suggests non-inferiority and equipoise."
When us doom and gloomers talk about the declining indications for radiation it's because of things like this. We're perpetually one successful chemo regimen away from becoming obsolete in an entire disease site. Historical clinical trials would say "FLOT/MAGIC were not superior to CROSS and thus CROSS should remain the standard of care." Unfortunately, nowadays the goalposts have shifted to "non-inferiority" and because of the pressures for academics to publish positive studies we have garbage like this where every metric reported by this abstract other than OS is numerically superior for CROSS and the conclusion is "the data suggests equipoise."
Background: The optimum combination curative approach to locally advanced adenocarcinoma of the esophagus and esophago-gastric junction (AEG) is unknown. A key question is whether neoadjuvant multimodal therapy, specifically CROSS (carboplatin/paclitaxel, 41.4Gy radiation therapy), is superior to optimum peri-operative chemotherapeutic regimens including modified MAGIC (epirubicin, cisplatin (oxaliplatin), 5-FU (capecitabine)) and more latterly FLOT (docetaxel, 5-FU, leucovorin, oxaliplatin). Neo-AEGIS was designed as the first randomised controlled trial to address this question.
Methods: 377 patients with cT2-3N0-3M0 AEG were randomly assigned to CROSS or peri-operative chemotherapy (ECF/ECX/EOF/EOX pre-2018, FLOT option 2019/20) at 24 sites (Ireland, UK, Denmark, France, Sweden). The primary outcome was overall survival. The initial power calculation was based on CROSS superiority of 10%. This was modified after the first futility analysis (70 events) to a non-inferiority margin of 5%. Secondary end points included toxicity, pathologic measures of response, and postoperative complications as per the Esophageal Complications Consensus Group (ECCG) definitions and Clavien-Dindo severity grade.
Results: Of 362 evaluable patients, 178 CROSS, 184 MAGIC/FLOT (157/27), 90% were male, median (range) age 64 (35-83), 84% were cT3, and 58% cN1. At a median (range) follow up of 24.5 (1-92) months, at the second futility analysis (60% of planned events), there were 143 deaths, 70 CROSS and 73 MAGIC/FLOT arm, with 3-year estimated survival probability of 56% (95% CI 47,64) and 57% (95% CI 48,65), respectively [(HR 1.02 (95%CI. 0.74-1.42))]. Based on the absence of futility evidenced in this data the DSMB recommended closure of recruitment in December 2020.
Conclusions: This RCT reveals no evidence that peri-operative chemotherapy is unacceptably inferior to multimodal therapy, notwithstanding greater proxy markers of local tumour response in the CROSS arm. Oncologic and operative outcomes were consistent with optimum modern benchmarks. These data strongly suggest non-inferiority and support equipoise in decision making in modern practice
 www.medpagetoday.com
www.medpagetoday.com
Just look at the first line of the article reporting this study:
"Perioperative chemotherapy in locally advanced esophageal or gastroesophageal junction (GEJ) adenocarcinoma was not "unacceptably" inferior to neoadjuvant chemoradiotherapy, an interim analysis of the randomized Neo-AEGIS trial suggested."
We're really in the ****ter when "not unacceptably inferior" is the benchmark for changing the standard of care.
When us doom and gloomers talk about the declining indications for radiation it's because of things like this. We're perpetually one successful chemo regimen away from becoming obsolete in an entire disease site. Historical clinical trials would say "FLOT/MAGIC were not superior to CROSS and thus CROSS should remain the standard of care." Unfortunately, nowadays the goalposts have shifted to "non-inferiority" and because of the pressures for academics to publish positive studies we have garbage like this where every metric reported by this abstract other than OS is numerically superior for CROSS and the conclusion is "the data suggests equipoise."
Background: The optimum combination curative approach to locally advanced adenocarcinoma of the esophagus and esophago-gastric junction (AEG) is unknown. A key question is whether neoadjuvant multimodal therapy, specifically CROSS (carboplatin/paclitaxel, 41.4Gy radiation therapy), is superior to optimum peri-operative chemotherapeutic regimens including modified MAGIC (epirubicin, cisplatin (oxaliplatin), 5-FU (capecitabine)) and more latterly FLOT (docetaxel, 5-FU, leucovorin, oxaliplatin). Neo-AEGIS was designed as the first randomised controlled trial to address this question.
Methods: 377 patients with cT2-3N0-3M0 AEG were randomly assigned to CROSS or peri-operative chemotherapy (ECF/ECX/EOF/EOX pre-2018, FLOT option 2019/20) at 24 sites (Ireland, UK, Denmark, France, Sweden). The primary outcome was overall survival. The initial power calculation was based on CROSS superiority of 10%. This was modified after the first futility analysis (70 events) to a non-inferiority margin of 5%. Secondary end points included toxicity, pathologic measures of response, and postoperative complications as per the Esophageal Complications Consensus Group (ECCG) definitions and Clavien-Dindo severity grade.
Results: Of 362 evaluable patients, 178 CROSS, 184 MAGIC/FLOT (157/27), 90% were male, median (range) age 64 (35-83), 84% were cT3, and 58% cN1. At a median (range) follow up of 24.5 (1-92) months, at the second futility analysis (60% of planned events), there were 143 deaths, 70 CROSS and 73 MAGIC/FLOT arm, with 3-year estimated survival probability of 56% (95% CI 47,64) and 57% (95% CI 48,65), respectively [(HR 1.02 (95%CI. 0.74-1.42))]. Based on the absence of futility evidenced in this data the DSMB recommended closure of recruitment in December 2020.
Conclusions: This RCT reveals no evidence that peri-operative chemotherapy is unacceptably inferior to multimodal therapy, notwithstanding greater proxy markers of local tumour response in the CROSS arm. Oncologic and operative outcomes were consistent with optimum modern benchmarks. These data strongly suggest non-inferiority and support equipoise in decision making in modern practice
Perioperative Chemo Enough in Esophageal Cancer?
MAGIC/FLOT regimens yielded similar overall survival to multimodal CROSS regimen
Just look at the first line of the article reporting this study:
"Perioperative chemotherapy in locally advanced esophageal or gastroesophageal junction (GEJ) adenocarcinoma was not "unacceptably" inferior to neoadjuvant chemoradiotherapy, an interim analysis of the randomized Neo-AEGIS trial suggested."
We're really in the ****ter when "not unacceptably inferior" is the benchmark for changing the standard of care.
