i hate that conversation. when its lumbar, you can nibble around the edges, but cervical myelopathy is different. it is tough to tell a patient they need surgery when you arent the one doing it.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Pictures of the Week
- Thread starter Epidural
- Start date
- Joined
- May 30, 2010
- Messages
- 1,651
- Reaction score
- 1,607
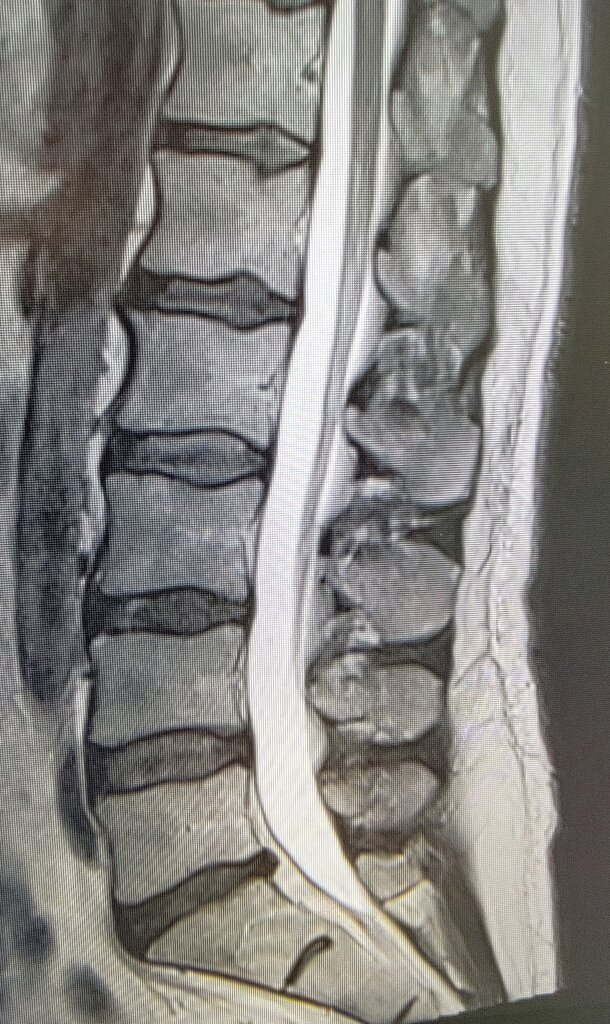
30 year old servicemember, 9/10 radicular pain crying during interview and can barely move, hasn't slept in weeks. Primary care mid-level waited 4 months to refer after percocet didn't work. Patient has been driving to work every day pulling over every 5-10 minutes this entire time.
Attachments
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
Transplant disc into PCP.30 year old servicemember, 9/10 radicular pain crying during interview and can barely move, hasn't slept in weeks. Primary care mid-level waited 4 months to refer after percocet didn't work. Patient has been driving to work every day pulling over every 5-10 minutes this entire time.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
I've said that during a P2P.Transplant disc into PCP.
Transplant disc into PCP.
mid-level, not PCP
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
Big enough to share.mid-level, not PCP
- Joined
- May 30, 2010
- Messages
- 1,651
- Reaction score
- 1,607
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
I’ve posted pics of this patient in the past. Updated films. Ribs hitting hips. Has MBA. Cannot work in office setting due to infection risk. Limited ambulation. Lungs not so good.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
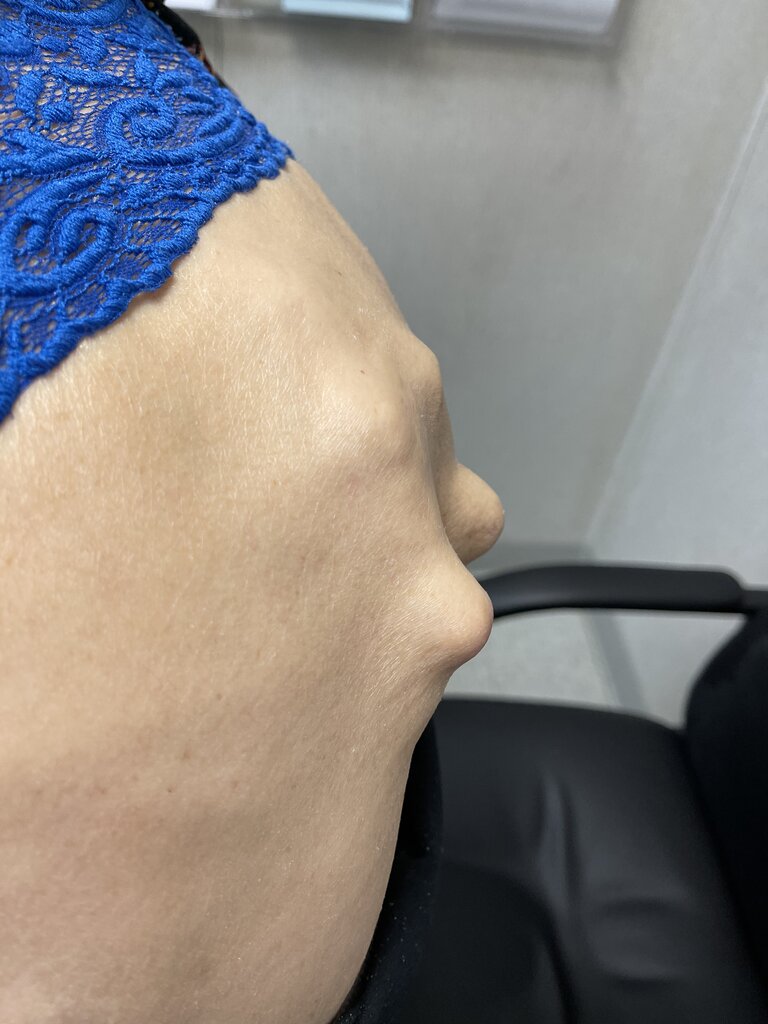
Need help. 5 prior back surgeries. 80 yrs old. Needs fabricated brace pillow type device to pad thoracolumbar junction deformity. Worsening scoliosis. P&O clinic?

- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,638
A little chiropractic ought to straighten that right out.View attachment 332837
View attachment 332838
I’ve posted pics of this patient in the past. Updated films. Ribs hitting hips. Has MBA. Cannot work in office setting due to infection risk. Limited ambulation. Lungs not so good.
- Joined
- Mar 22, 2008
- Messages
- 3,540
- Reaction score
- 2,163
Steve’s patient population never ceases to amaze. SMfH
Need help. 5 prior back surgeries. 80 yrs old. Needs fabricated brace pillow type device to pad thoracolumbar junction deformity. Worsening scoliosis. P&O clinic?
View attachment 332839View attachment 332840
this doesnt even look human. its a decubitus waiting to happen. you will need a custom chair with essentially a cutout for the low back. maybe something like a Roho cushion for the back. i'm not sure your typical O&P could handle it, but a place with a lot of SCI patients could.
- Joined
- Jan 2, 2016
- Messages
- 2,100
- Reaction score
- 2,076
Vertical Tush Cush?this doesnt even look human. its a decubitus waiting to happen. you will need a custom chair with essentially a cutout for the low back. maybe something like a Roho cushion for the back. i'm not sure your typical O&P could handle it, but a place with a lot of SCI patients could.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
Called Hanger P&O today. I will get them the Xray to look at so they can build the right multidensity foam back off-loader.
Yup, remember, in AP the screws are outside the spinal canal. She makes a 90 degree turn at the junctional kyphosis. The top two screws are not in a bone, maybe in some bon material. The 2nd set down from the top are amazingly even with a cage. Broken screw in S1.
Pain controlled on oxy 15 tid, failed SCS (easy to get in- straight down was straight up the canal). Ambulatory with rolling walker. Needs setup/standby for ADLs.
Yup, remember, in AP the screws are outside the spinal canal. She makes a 90 degree turn at the junctional kyphosis. The top two screws are not in a bone, maybe in some bon material. The 2nd set down from the top are amazingly even with a cage. Broken screw in S1.
Pain controlled on oxy 15 tid, failed SCS (easy to get in- straight down was straight up the canal). Ambulatory with rolling walker. Needs setup/standby for ADLs.
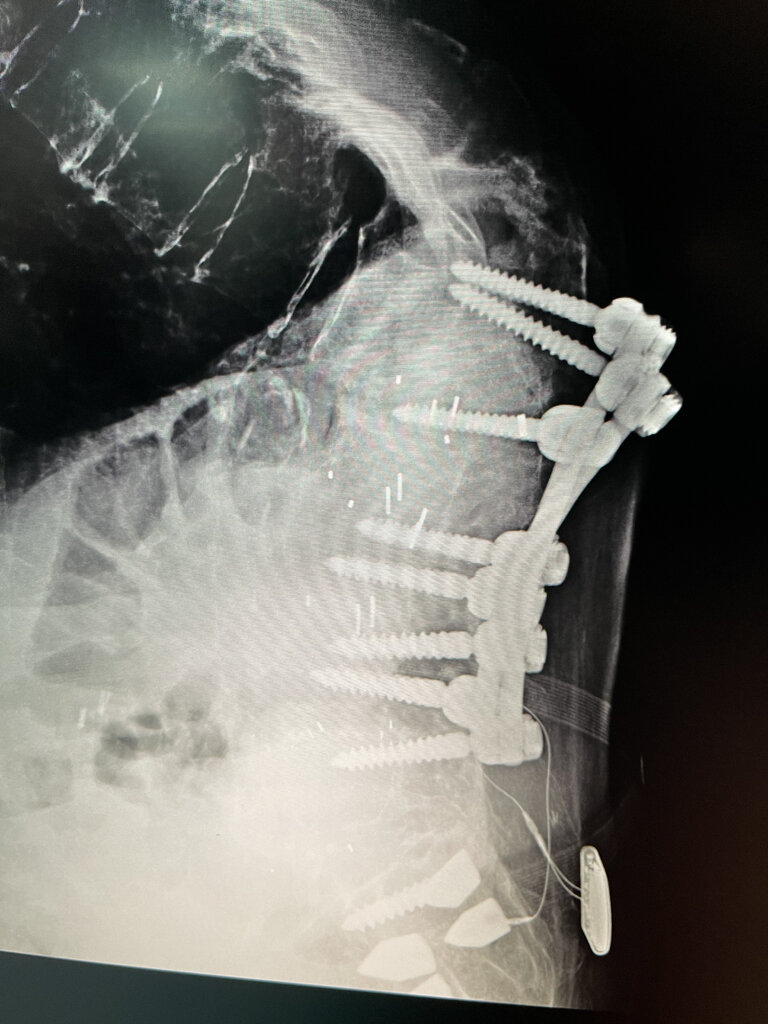
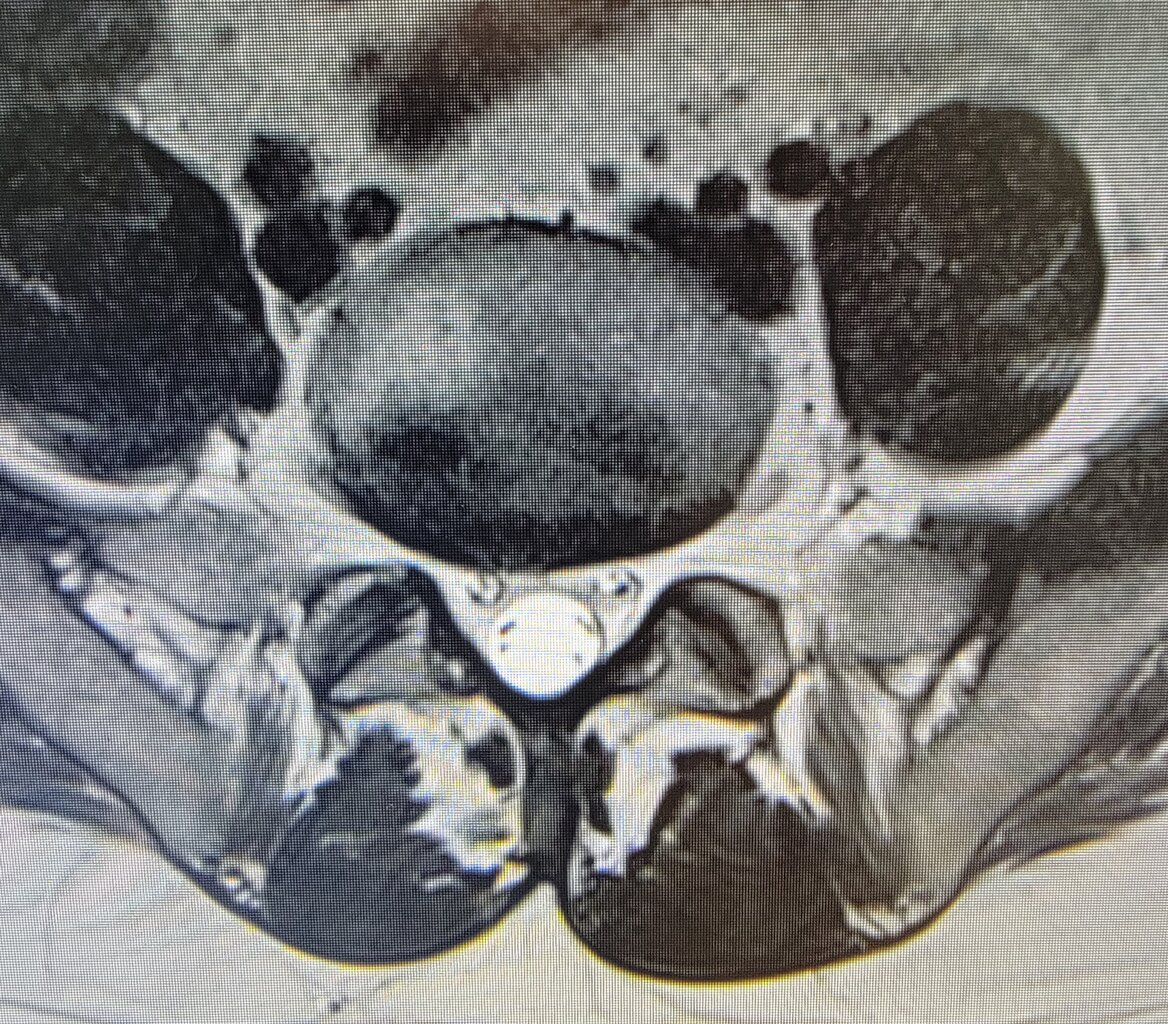
Cervical facet cyst. I’ve seen a lot of lumbar facet cysts but never cervical.

New onset RUE pain/tingling increasing over the past month. Has had RF in past, most recently last fall.
I rarely do PO steroids, but sent some in for him.
Any utility in cesi? All articles pertaining to cervical facet cyst seemed to end in surgical intervention. Patient is hoping to avoid surgery. Pain is severe, per patient his strength is maintained.
New onset RUE pain/tingling increasing over the past month. Has had RF in past, most recently last fall.
I rarely do PO steroids, but sent some in for him.
Any utility in cesi? All articles pertaining to cervical facet cyst seemed to end in surgical intervention. Patient is hoping to avoid surgery. Pain is severe, per patient his strength is maintained.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
Surgery or suffer.Cervical facet cyst. I’ve seen a lot of lumbar facet cysts but never cervical.
View attachment 333099
View attachment 333100
New onset RUE pain/tingling increasing over the past month. Has had RF in past, most recently last fall.
I rarely do PO steroids, but sent some in for him.
Any utility in cesi? All articles pertaining to cervical facet cyst seemed to end in surgical intervention. Patient is hoping to avoid surgery. Pain is severe, per patient his strength is maintained.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
IMO, it wouldn't be wrong to do a CESI while you're waiting on the referral process to take place considering surgery won't happen the day of the consult.
could try to aspirate but i wouldnt inject anything or pressurize/pop it.
this is an instance where an aggressive injectionist (not me) might try a C5 TFESI if the patient was adamantly against surgery or wasnt a candidate medically.
this is probably going to the OR
this is an instance where an aggressive injectionist (not me) might try a C5 TFESI if the patient was adamantly against surgery or wasnt a candidate medically.
this is probably going to the OR
- Joined
- Feb 1, 2005
- Messages
- 4,899
- Reaction score
- 1,882
No weakness, not myelopathic, not chronic, patient prefers no surgery.... I aspirate and inject. If no No better or recurrent... see surgeon
Thanks guys. I thought this was pretty interesting to see.
I may try a CESI if he is interested From the looks of that facet joint on MRI, I am doubtful I can get a needle in there- absolutely no joint space!
The surgeons I am thinking of sending him to are not overly aggressive
I may try a CESI if he is interested From the looks of that facet joint on MRI, I am doubtful I can get a needle in there- absolutely no joint space!
The surgeons I am thinking of sending him to are not overly aggressive
- Joined
- May 30, 2010
- Messages
- 1,651
- Reaction score
- 1,607
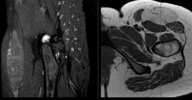
Young female servicemember with atraumatic left hip pain and lateral thigh parasthesia
So just a bit more background since I think its an interesting case.
Patient went in to PCM about a year ago with thigh pain and numbers, gets referred to PT but gradually worsens. They get imaging and it shows this big thigh tumor causing local mass effect on the surrounding tissues. Rads reads it as potential sarcoma, so she gets a wide excision biopsy. It turns out it's a super rare brown fat tumor called a hibernoma. It appears that the LFCN was either enveloped in it or got bagged during the surgery, because now she's completely hypoesthetic in the LFCN distribution. She still has some pain which I think is more intraarricular, so going to try a hip injection. I thought it was an interesting etiology for meralgia parasthetica, gave it to a student to make a poster about it.
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
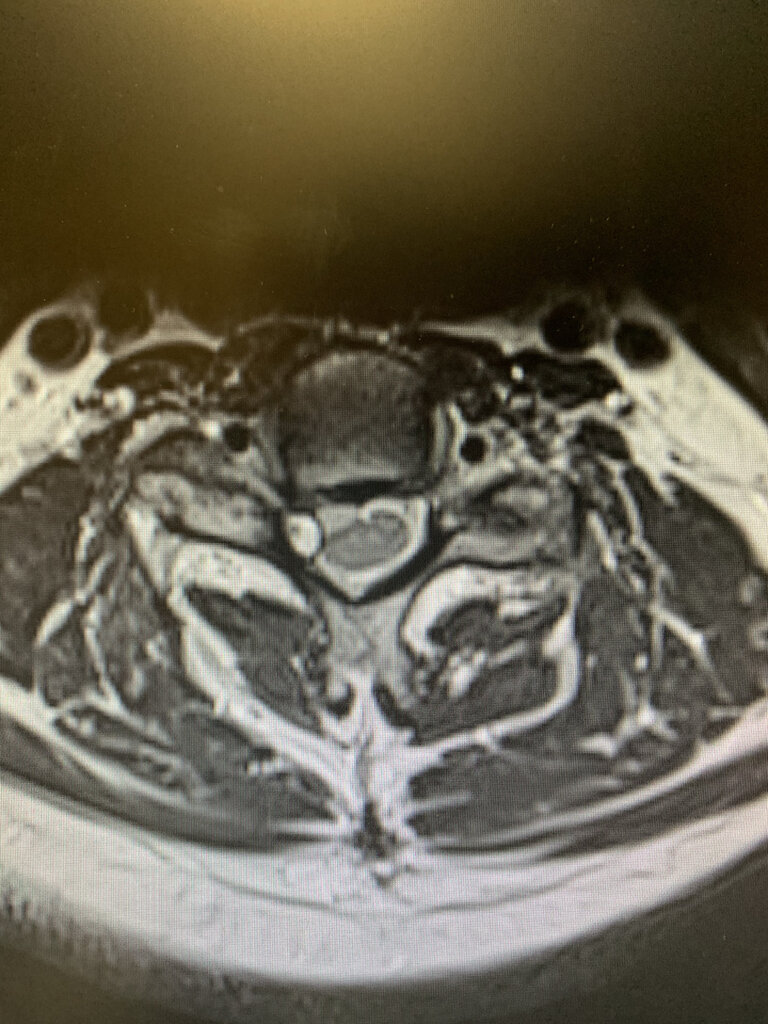
sometimes its not what everyone thinks it is that is causing the pain. referred by PCP for severe back pain radiating down the left leg that oxy 5 mg 6 a day is not covering.
elderly male, multiple medical problems, including severe heart disease and is being evaluated for LVAD. worsening over past 3 years, to the point now he is bedbound from pain and heart disease. diabetic on 3 agents and insulin, and on multiple cardiac meds including milrinone iv infusion at home.
long history of back pain, s/p fusion L45 roughly 5 years ago. didn't seem to help. seen by neurosurgeon - no surgery to recommend. referred to pain management for possible injections. patient never went. of note, patient chronically anticoagulated and cardiologist would not approve stopping
also long history of hip pain bilateral, and has had several "hip injections" by ortho, which on review appear to be GT injections. they would help a little bit for 5-6 weeks at best. not a candidate for further hip surgery because of severe heart disease.
very difficult getting patient to office. missed first appointment because he could not get in. did come in to second appointment in wheelchair. refused to get out of wheelchair due to pain. unable to flex forward due to pain and back examination revealed well healed scar with scoliotic deformity. severe pain with forward flexion. limited hip examination due to being in wheelchair, but patient refused internal and external rotation of hip.
elderly male, multiple medical problems, including severe heart disease and is being evaluated for LVAD. worsening over past 3 years, to the point now he is bedbound from pain and heart disease. diabetic on 3 agents and insulin, and on multiple cardiac meds including milrinone iv infusion at home.
long history of back pain, s/p fusion L45 roughly 5 years ago. didn't seem to help. seen by neurosurgeon - no surgery to recommend. referred to pain management for possible injections. patient never went. of note, patient chronically anticoagulated and cardiologist would not approve stopping
also long history of hip pain bilateral, and has had several "hip injections" by ortho, which on review appear to be GT injections. they would help a little bit for 5-6 weeks at best. not a candidate for further hip surgery because of severe heart disease.
very difficult getting patient to office. missed first appointment because he could not get in. did come in to second appointment in wheelchair. refused to get out of wheelchair due to pain. unable to flex forward due to pain and back examination revealed well healed scar with scoliotic deformity. severe pain with forward flexion. limited hip examination due to being in wheelchair, but patient refused internal and external rotation of hip.
sometimes its not what everyone thinks it is that is causing the pain. referred by PCP for severe back pain radiating down the left leg that oxy 5 mg 6 a day is not covering.
elderly male, multiple medical problems, including severe heart disease and is being evaluated for LVAD. worsening over past 3 years, to the point now he is bedbound from pain and heart disease. diabetic on 3 agents and insulin, and on multiple cardiac meds including milrinone iv infusion at home.
long history of back pain, s/p fusion L45 roughly 5 years ago. didn't seem to help. seen by neurosurgeon - no surgery to recommend. referred to pain management for possible injections. patient never went. of note, patient chronically anticoagulated and cardiologist would not approve stopping
also long history of hip pain bilateral, and has had several "hip injections" by ortho, which on review appear to be GT injections. they would help a little bit for 5-6 weeks at best. not a candidate for further hip surgery because of severe heart disease.
very difficult getting patient to office. missed first appointment because he could not get in. did come in to second appointment in wheelchair. refused to get out of wheelchair due to pain. unable to flex forward due to pain and back examination revealed well healed scar with scoliotic deformity. severe pain with forward flexion. limited hip examination due to being in wheelchair, but patient refused internal and external rotation of hip.
View attachment 333778View attachment 333779View attachment 333780
I assume he can’t get surgery since he can’t stop blood thinners... what’s your plan?
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
my plan it to talk to everyone in the world.
MRI hip:
hard to pick any 1 image, but...
he had avascular necrosis of the left femoral head with subchondral collapse and multiple sacral insufficiency fractures.
MRI hip:
hard to pick any 1 image, but...
he had avascular necrosis of the left femoral head with subchondral collapse and multiple sacral insufficiency fractures.
articular branch RF for the hip has been my go to in these cases to help as can do that safely on anticoagulation, the SI insufficiency fractures would be harder, med adjustment obviouslymy plan it to talk to everyone in the world.
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
it took 6 weeks to get that MRI. I did break down and start him on fentanyl patch temporarily, family was in process of setting up home hospice, but they okayed to try fentanyl and get MRI. didn't help much. knocked him out, so that ended my palliative care treatment with opioids.
COVID hit so i couldnt get him in the office for any injections at all. in fact, after that 1st appointment, the rest were all virtual.
on top of all this, his wife died of COVID but he never caught it.
after MRI, I contacted the cardiologist who - thankfully - really believes in QoL and we both agreed - home hospice vs. intraoperative death seemed not that different in end result so he said if anesthesiology would allow, he would "approve", and put him in SICU post op.
anesthesiology said ASA 4, but of course, we can do it.
then contacted ortho, who said okayyy.....
told patient to contact ortho, and that is the last I heard from him.
patient had hip replacement 10 months ago. had a little rocky post op course (pneumonia) but pain was apparently gone POD2 onwards. still has other issues, and he is a permanent resident of a nursing home now apparently but is ambulatory. per Ortho "phenomenal clinical response"
I post now because stupid EMR wanted me to delete a lab test I had ordered a year ago.
COVID hit so i couldnt get him in the office for any injections at all. in fact, after that 1st appointment, the rest were all virtual.
on top of all this, his wife died of COVID but he never caught it.
after MRI, I contacted the cardiologist who - thankfully - really believes in QoL and we both agreed - home hospice vs. intraoperative death seemed not that different in end result so he said if anesthesiology would allow, he would "approve", and put him in SICU post op.
anesthesiology said ASA 4, but of course, we can do it.
then contacted ortho, who said okayyy.....
told patient to contact ortho, and that is the last I heard from him.
patient had hip replacement 10 months ago. had a little rocky post op course (pneumonia) but pain was apparently gone POD2 onwards. still has other issues, and he is a permanent resident of a nursing home now apparently but is ambulatory. per Ortho "phenomenal clinical response"
I post now because stupid EMR wanted me to delete a lab test I had ordered a year ago.
D
deleted875186
Seems reasonable to try a THA to be honest, some of these LVAD patients are pretty stable, although the Milrinone is a bit worrisome. His QOL is so bad that I think it was worth doing.it took 6 weeks to get that MRI. I did break down and start him on fentanyl patch temporarily, family was in process of setting up home hospice, but they okayed to try fentanyl and get MRI. didn't help much. knocked him out, so that ended my palliative care treatment with opioids.
COVID hit so i couldnt get him in the office for any injections at all. in fact, after that 1st appointment, the rest were all virtual.
on top of all this, his wife died of COVID but he never caught it.
after MRI, I contacted the cardiologist who - thankfully - really believes in QoL and we both agreed - home hospice vs. intraoperative death seemed not that different in end result so he said if anesthesiology would allow, he would "approve", and put him in SICU post op.
anesthesiology said ASA 4, but of course, we can do it.
then contacted ortho, who said okayyy.....
told patient to contact ortho, and that is the last I heard from him.
patient had hip replacement 10 months ago. had a little rocky post op course (pneumonia) but pain was apparently gone POD2 onwards. still has other issues, and he is a permanent resident of a nursing home now apparently but is ambulatory. per Ortho "phenomenal clinical response"
I post now because stupid EMR wanted me to delete a lab test I had ordered a year ago.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
New patient to me. Procedure note from 2013 done elsewhere. I've shared a similar note a few years back. Must have good insurance.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
The part in the epidural space at T8 has 10 contacts. It is a 5x4 array. But still.
what about the SI joint? why was that not injected?View attachment 334193
New patient to me. Procedure note from 2013 done elsewhere. I've shared a similar note a few years back. Must have good insurance.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
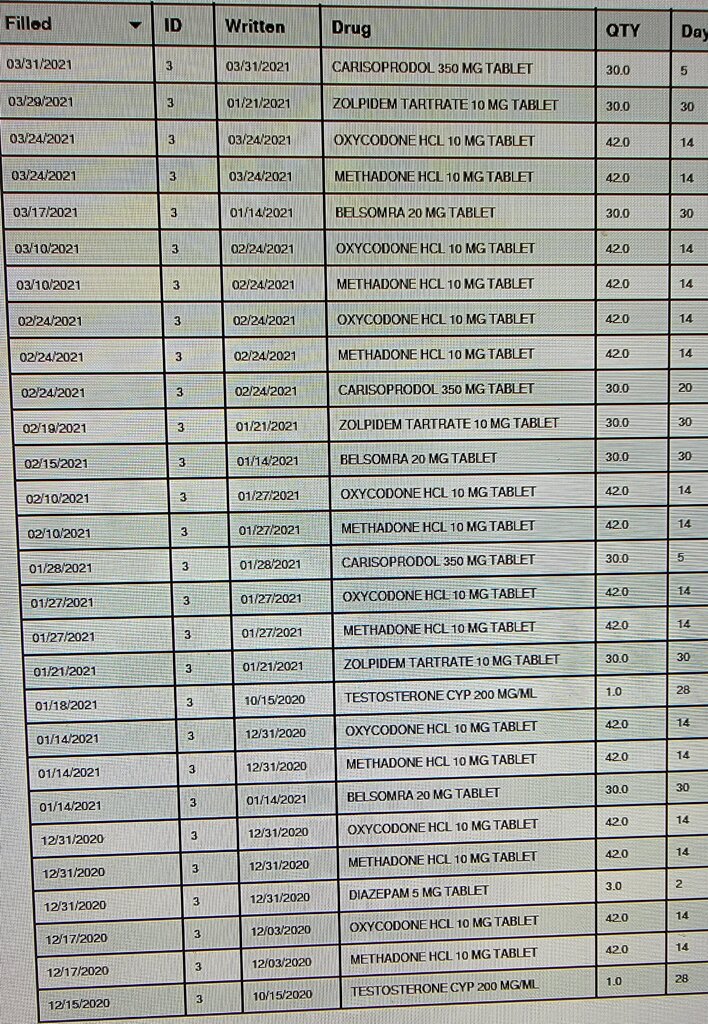
My 9 AM is coming in for a NPV and discussion about potential SCS trial.
That is the worst of it right there...
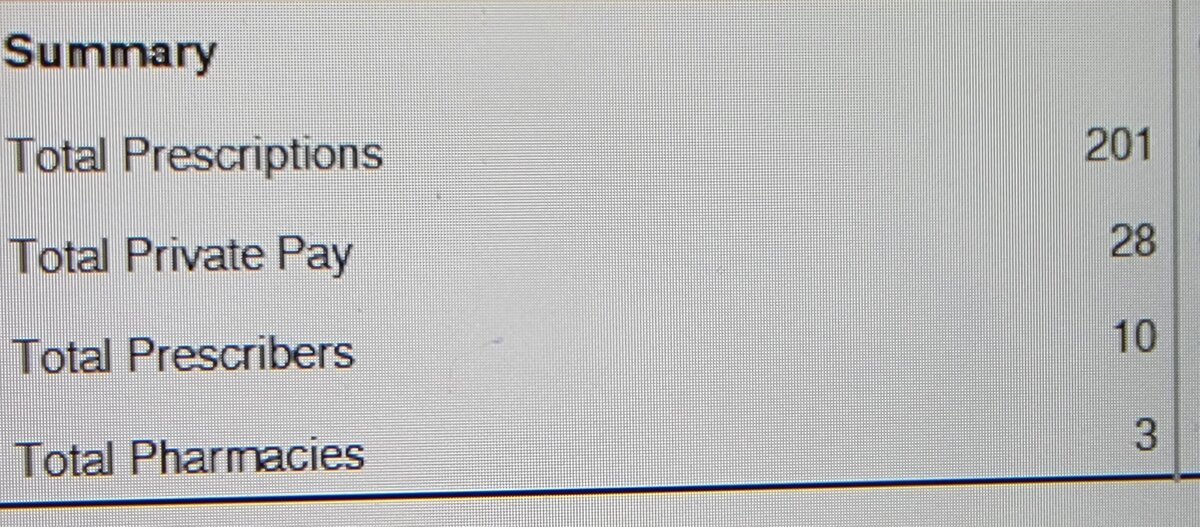
I am sure this visit will be comfortable and pleasing.
That is the worst of it right there...
I am sure this visit will be comfortable and pleasing.
- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,638
There was a big article in the Associated Press a few years ago about trying to force people off opioids using SCS and how terrible it was, featuring a guy who had carved “death row” into his headboard. Just print it out and give it to the patient - I did once.My 9 AM is coming in for a NPV and discussion about potential SCS trial.
View attachment 334635View attachment 334636
That is the worst of it right there...
View attachment 334637View attachment 334638
I am sure this visit will be comfortable and pleasing.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
...and that was great. I had to carry my bookbag with me into the next patient room (I carry in my bookbag) bc of this dude.
WTH
Methadone 16 yrs now, started for cramps at 29 yo.
Demanding Soma.
"No follow up with me."
No physical exam.
WTH
Methadone 16 yrs now, started for cramps at 29 yo.
Demanding Soma.
"No follow up with me."
No physical exam.
- Joined
- May 8, 2004
- Messages
- 4,004
- Reaction score
- 1,633
so what do you bill for this waste of your time?...and that was great. I had to carry my bookbag with me into the next patient room (I carry in my bookbag) bc of this dude.
WTH
Methadone 16 yrs now, started for cramps at 29 yo.
Demanding Soma.
"No follow up with me."
No physical exam.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
203so what do you bill for this waste of your time?
I spent 25 min with him before he turned into an idiot. His pain doctor refuses to Rx Soma, so one of our shoulder guys gave him 3 Rx for it for some stupid F'ing reason.
Our shoulder guy didn't check his PDMP and had no clue he's on opiates.
We got to that part of the discussion and I straight told him Soma isn't a medication I prescribe and the tantrum started.
- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,638
Latest entry in my “always review your own imaging” files. 82yo M with dementia, referred for back and right leg pain. Most of the history came from his wife - he would give appropriate but generally 1-3 word answers. Long history of back pain. MRI from December 2020 showed age-typical degenerative changes, old T12 fracture. Of course some lower lumbar DDD and foraminal narrowing that could account for the pain. Did an ESI, and he came back with no improvement, with the interval addition of a recent fall. X ray stable but complaining of worsening back pain so ordered a new MRI to evaluate for acute fracture. Image as follows. Missed on the initial read but when I called back and talked to a radiologist (not the one who read it initially) he said likely psoas abscess from a ruptured diverticulum. Less likely malignancy given the 12/20 MRI was totally normal in that area.
- Joined
- Dec 13, 2005
- Messages
- 5,316
- Reaction score
- 3,595
Why a level 3? That is a level 5 always if you have to carry your gun with you. Life saving decision making.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
Not sure how to defend that level of coding TBH. He was a complete idiot, but how do you code for that? Dude made me nervous - Polypharmacy with a low IQ, definite psychological issues and his wife is present (he has to show her he's not scared to tell me what's up)...He's wearing a flat brim hat (pet peeve of mine on several levels) and a face mask while pacing around the room.Why a level 3? That is a level 5 always if you have to carry your gun with you.
Made me nervous but I don't know what the terminology is for that to support a 205.
- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,638
You discussed life-threatening combination of medications, independently reviewed imaging, reviewed PDMP, and reviewed past notes, so if he’s Medicare you should be able to bill a high complexity level. If he’s on any other insurance though, still using the older E&M standards, if didn’t do a comprehensive physical exam you’d be limited to a level 3. I’ve run into that before myself with that type of patient.Not sure how to defend that level of coding TBH. He was a complete idiot, but how do you code for that? Dude made me nervous - Polypharmacy with a low IQ, definite psychological issues and his wife is present (he has to show her he's not scared to tell me what's up)...He's wearing a flat brim hat (pet peeve of mine on several levels) and a face mask while pacing around the room.
Made me nervous but I don't know what the terminology is for that to support a 205.
- Joined
- Jul 25, 2008
- Messages
- 2,058
- Reaction score
- 455
204?Not sure how to defend that level of coding TBH. He was a complete idiot, but how do you code for that? Dude made me nervous - Polypharmacy with a low IQ, definite psychological issues and his wife is present (he has to show her he's not scared to tell me what's up)...He's wearing a flat brim hat (pet peeve of mine on several levels) and a face mask while pacing around the room.
Made me nervous but I don't know what the terminology is for that to support a 205.
U could prob bill it just on time - these patients take forever.
I always bill 204 with a new patient - you review medical records, PDMP, explain disease process, discuss r/b of opioids if prescribing them, discuss a procedure if your going to submit for it.
- Joined
- Apr 20, 2018
- Messages
- 2,168
- Reaction score
- 1,659
No physical exam was done - I documented, "No physical exam. Pt paced throughout the visit and was highly agitated and accusatory. Unpleasant and tried to walk out midsentence." That was basically my PE.You discussed life-threatening combination of medications, independently reviewed imaging, reviewed PDMP, and reviewed past notes, so if he’s Medicare you should be able to bill a high complexity level. If he’s on any other insurance though, still using the older E&M standards, if didn’t do a comprehensive physical exam you’d be limited to a level 3. I’ve run into that before myself with that type of patient.
- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,638
Similar experience for me was the guy who screamed “just give me some f***ing drugs!”. Shortly before storming out because I wouldn’t.No physical exam was done - I documented, "No physical exam. Pt paced throughout the visit and was highly agitated and accusatory. Unpleasant and tried to walk out midsentence." That was basically my PE.
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
there are ways of documenting an examination that can make you comfortable with a level III or IV code that is not time dependent, in these circumstances. personal experience. may not want to include purple phrasesNo physical exam was done - I documented, "No physical exam. Pt paced throughout the visit and was highly agitated and accusatory. Unpleasant and tried to walk out midsentence." That was basically my PE.
HEENT: NC/AT. PERRL. conjunctivae injected and blood filled when denied opioid script.
no obvious facial swelling. hearing intact. full range of motion of cervical spine 180 degrees.
Cor: good color of extremities. no visible carotid pulsations. not cyanotic nor diaphoretic. excellent carotid bloodflow as he stormed out.
Lungs: Good airflow without audible wheezing. initially not tachypneic. no audible wheezing. no splinting. pulmonary volumes appropriate and able to swear loudly without breath intake for over 90 seconds.
Abd: not actively vomiting. does not appear nauseous. abdomen not distended on superficial examination.
Motor: moves all extremities without limitations. middle finger extends to zero degrees with no difficulty.
Neuro: CN II-XII intact. motor intact, and no obvious paralysis. no cerebellar signs.
Derm: no visible rash. F#$% You tattoo visible left forearm. No obvious lymphedema
Psych: A+Ox3. affect belligerent. insight extremely poor and focused on opioids. mood angry. memory short term intact. speech not slurred mostly coherent except when he was screaming. use of swear words were contextually appropriate.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
Little something off of twitter. 2 level discogram.
because more surgery must help. Ugh
That's only slick if they did it from an anterior approach.Little something off of twitter. 2 level discogram.
because more surgery must help. Ugh
- Joined
- May 30, 2006
- Messages
- 201
- Reaction score
- 119
Steve and I must see the same LinkedIn feeds, because I saw the same post, and I pretty sure they did use an anterior approach for the discogram.That's only slick if they did it from an anterior approach.
I just started following some pain guys on LinkedIn and it’s...interesting. It’s 99% pain guys and device reps clapping each other on the back for how much hardware they can put in a patient’s spine. And often the x-rays look otherwise pretty normal.
- Joined
- Oct 7, 2011
- Messages
- 14,652
- Reaction score
- 5,953
I don't see the SIJ fusions on that image.
so there is more work to be done.
so there is more work to be done.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
Sent for SCS trial and implant.
- Joined
- May 30, 2005
- Messages
- 21,249
- Reaction score
- 12,361
So I can go today and follow up for MRI. Cord signal change consistent with Milo malacia T 11 to 12 multilevel degenerative changes with post laminectomy syndrome lumbar spine. I look at his scar and everything looks good from the outside after the visit his wife asked me to look at his shoulder. This is what I found.
Attachments
Similar threads
- Replies
- 21
- Views
- 810