Story time! (It’s a long one, but lots of pictures) showing evolution of discitis.
Patient with history of chronic back pain, prior improvement with injections, and Hx of lung cancer and pacemaker presented to my partner as well as to ER several times with new severe (debilitating) back pain. CT scan shows significant degenerative changes, “severe multilevel lumbar spondylosis with erosive endplate changes at L2-3.”
Prior CT for lung cancer screening done 3/21
View attachment 339911
CT angio obtained in the ER 5/10/21 for “radiating chest pain and diffuse abdominal pain”
View attachment 339912
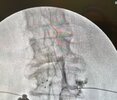
New CT lumbar obtained by my partner 6/14/21. Radiologist notes significant degenerative changes, “severe multilevel lumbar spondylosis with erosive endplate changes at L2-3.”
View attachment 339913
He then obtains a bone scan on 6/22 due to severity of the patient’s pain. The bone scan is read as moderate to severe osteoarthritis changes particularly at L2-3, with compression not excluded. Also gave him oxycodone at this point which did not touch the pain.
View attachment 339914
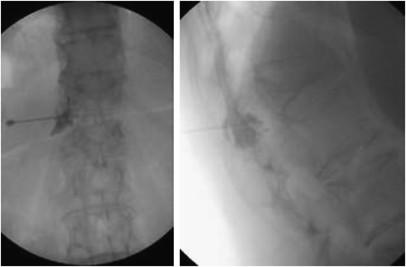
At this point. My partner asks me to see him for possible kyphoplasty. I review the imaging and agree to see the patient but also ask him to order WBC, ESR, and CRP as it doesn’t look quite right for a compression fracture. Patient sees me next day, still hasn’t had labs done. We discuss possible kypho - the guy is absolutely miserable from the back pain but denies any infectious symptoms. Prior WBC from one of his ER trips was normal. I tell him I need those labs first and we need a blood thinner clearance from his cardiologist.
Yesterday, labs come back. WBC 12.8, ESR 35, CRP 73.
I called him and told him he needed to go the the ER for new imaging, spine surgeon consultation, and likely biopsy and IV antibiotics. He fought it because they hadn’t helped him before but ultimately agreed.
CT scan in the ER reads discitis with surrounding cellulitis. Had CT-guided biopsy the next day.
View attachment 339915