Excellent post as always Blade.
I'm a Ca-1 right now, I often over hear "if this is Private practice this case would be done".
Obv the oral board answer is 7 days.
But let me pose the question: How many of yall out there in private practice would do this case if the pt was off it for 3 days with normal CrCl? (assume no neuroaxial and just do GA w/ ETT A line)
72hrs = 4.6 Half lives.
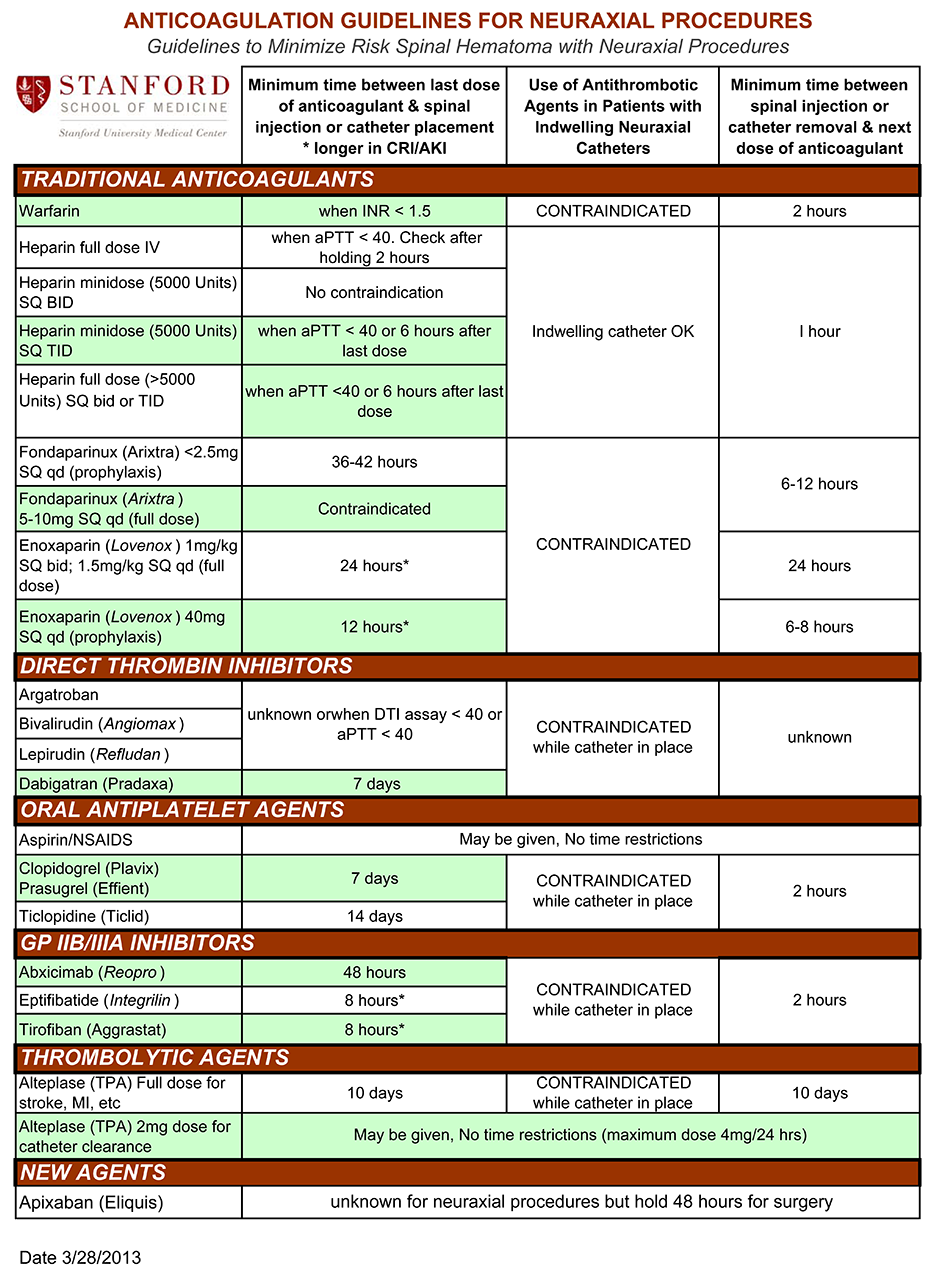
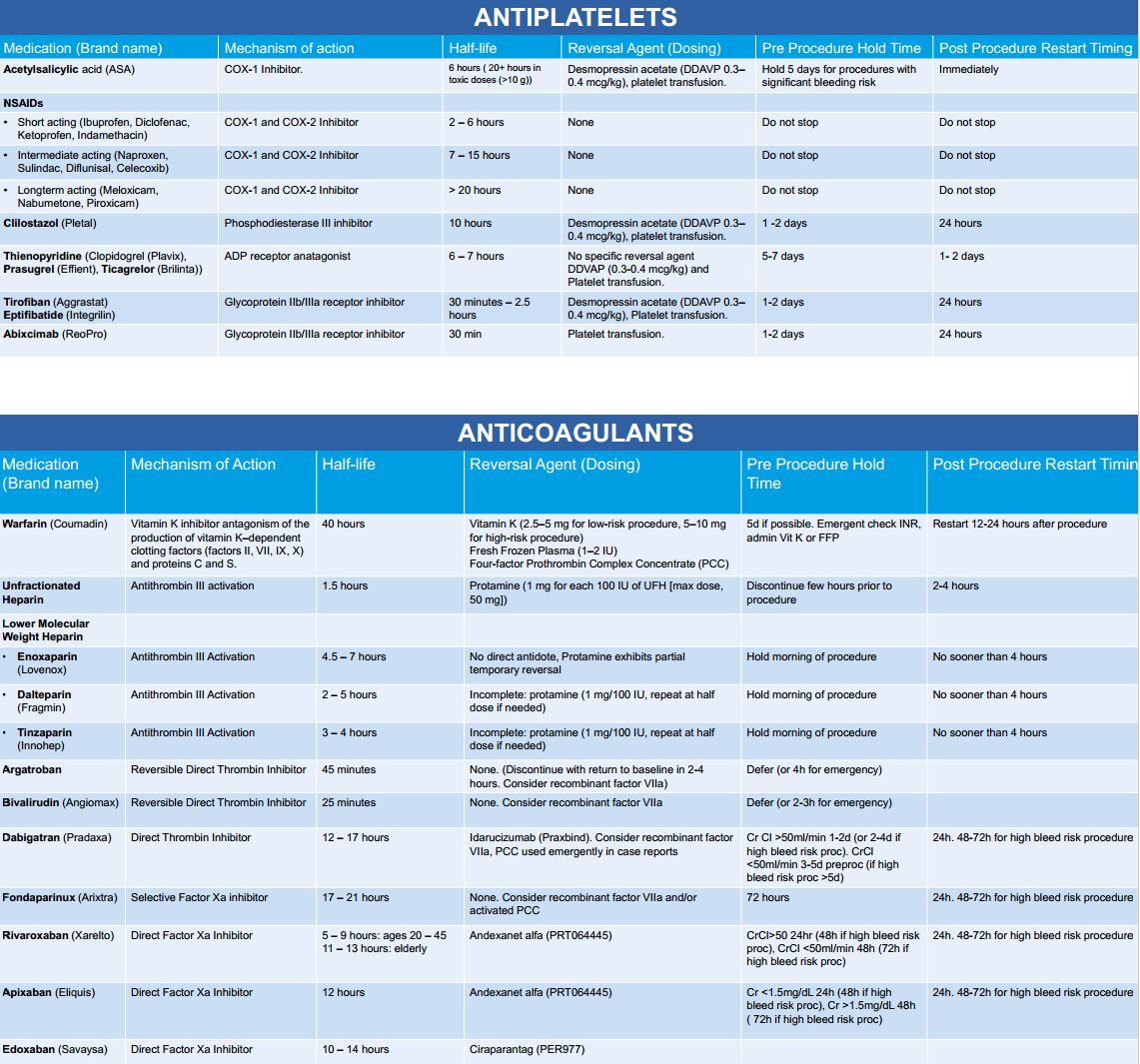
The board answer is definitely NOT 7 days. It's 5 days currently for NEURAXIAL anesthesia per the ASRA guidelines (
Anticoagulation 3rd Edition), though there's limited data here, so you could make an argument for longer. But that's for neuraxial anesthesia...for doing the case, I DEFINITELY wouldn't wait 7 days even with crappy renal function.
This case should be done in private practice and academic medical setting without issue.
If the patient has been off for a solid 5 days, repeat the labs and if coags are normal, I would personally place a spinal. For starters, spinal anesthesia for total joints has been decisively shown to reduce EBL in the perioperative period (among many other benefits). TXA is a no-brainer (we give it for all total joints where it's not contraindicated).
But if you're really worried about the spinal hematoma risk, do the case under GA, and there's no reason then to repeat coags.
But in my opinion, even with elevated coags, off pradaxa for 5 days, there's no reason to cancel this case.