I am a psychiatrist but have a question for pain management. If an individual gets repeated pulsed RFAs for a chronic neuropathy, what happens in the long term? Like say they get 2 a year for 5-20 years? Does the pain tend to get worse, better, or stay the same after these repeated procedures?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Prognosis for repeated pulsed RFAs
- Thread starter reader278
- Start date
- Status
- Not open for further replies.
Does that mean, there is no compounding therapeutic effect? And that sometimes people get worse from pulsed RFAs?
sounds like you must of gotten worse...
I haven't had a pulsed RFA. I likely have an inferior branch saphenous neuropathy post knee arthroscopy, and am looking into my various options. I've been referred for a diagnostic block from a pain physician who does genicular RFA, and just looking into my options, and risks and benefits. Having had a negative outcome post surgery, I'm just cautious about procedures now. Pulsed RFA seems promising, but I'm trying to figure out how viable it is to have these procedures repeatedly long term, and whether people may eventually not need them if their pain threshold resets or they are able to gain back enough strength and functioning that maybe when the pain returns it's less impairing? I have no idea, and can't seem to figure this out from a review of pubmed.
- Joined
- Oct 23, 2005
- Messages
- 7,209
- Reaction score
- 4,723
I haven't had a pulsed RFA. I likely have an inferior branch saphenous neuropathy post knee arthroscopy, and am looking into my various options. I've been referred for a diagnostic block from a pain physician who does genicular RFA, and just looking into my options, and risks and benefits. Having had a negative outcome post surgery, I'm just cautious about procedures now. Pulsed RFA seems promising, but I'm trying to figure out how viable it is to have these procedures repeatedly long term, and whether people may eventually not need them if their pain threshold resets or they are able to gain back enough strength and functioning that maybe when the pain returns it's less impairing? I have no idea, and can't seem to figure this out from a review of pubmed.
You said you are looking into various options. What are your other options?
Surgery already made you worse and surgery is 10X riskier than pulsed RFA, long term opioids are much riskier than pulsed RFA.
I expect your options are likely pulsed RFA or neuropathic meds. Certainly reasonable to try a few neuropathic meds first and if you fail them, then try pulsed RFA. I doubt you have many other options.
Pulsed RF is an odd cat but some swear by it. I haven't had great results from it but the nondestructive nature of it keeps me trying it when I don't want to destroy a nerve.
If you've got this concern, and medications aren't your cup of tea, start with a regular nerve block and see how it helps. A pulsed RF after that is a great option. Then consider finding someone who would try a peripheral nerve stimulator system if the pulsed RF doesn't last very long. A PNS system like the SPR Therapeutics Sprint might be a good test for you as this might be something that resolves if the nerve regenerates.
If you've got this concern, and medications aren't your cup of tea, start with a regular nerve block and see how it helps. A pulsed RF after that is a great option. Then consider finding someone who would try a peripheral nerve stimulator system if the pulsed RF doesn't last very long. A PNS system like the SPR Therapeutics Sprint might be a good test for you as this might be something that resolves if the nerve regenerates.
- Joined
- Jul 25, 2008
- Messages
- 2,058
- Reaction score
- 455
Why not just regular RF
Sent from my iPhone using SDN
Sent from my iPhone using SDN
Isn't conventional RFA less safe? I'm reading scary things like deafferentation pain.....I don't need more issues to add to the list haha. Question about the peripheral nerve stimulator SPRINT-it only lasts 60 days, what happens after that?
- Joined
- Aug 16, 2007
- Messages
- 5,379
- Reaction score
- 2,520
I don’t think we know the long term effects of repeated pulsed RF or standard RF for that matter. I’d try some neuropathic meds if you’re worried and then RF if that fails. Deafferentation pain is relatively rare. Maybe try a topical compounding cream that includes ketamine
I'm starting with physiotherapy plus already on gabapentin and duloxetine. To make matters worse, I'm 30 F married and want to have children soon, so I can't stay on the meds and not sure what to do. I figure it's either a nerve entrapment or a neuroma...
- Joined
- Mar 17, 2011
- Messages
- 148
- Reaction score
- 91
I would scrap pulsed RFA and just do a standard RFA. An alternative to this would be trialing some compound topical medication for the knees. I’ve had pretty good success using either or both RFA/cream. The creams usually are lidocaine/ketamine/gabapentin/ clonidine/diclofenac in some combo, or all of these. Definitely a safe option that would avoid oral meds and the s/e that can come along with them.
PT and CBT/DBT are the most useful.
The medications can help. Topical agents are a great option for this nerve specifically due to the relatively superficial nature of it.
Conventional RFA or pulsed RF are options. The peripheral nervous system does regenerate after a lesion, but my problem is that it isn't always perfect regeneration. In post-traumatic/surgical states where nerve trauma appears to have incited a pain state, my preference is to not cause more trauma with thermal ablation, although that's purely a theoretical concern as we do it all the time for facet joints, and this is a purely a sensory nerve we would be considering ablating. I prefer pulsed along with a nerve block as my first round of treatment, followed by PNS if needed/indicated before a conventional RFA.
The SPRINT system reportedly has long term benefits of over 12 months despite just 60 days of treatment. There are more durable implants out there if needed, both peripherally and at the level of the spinal cord/DRG.
A localized injection with ultrasound guidance can help delineate peripheral from centralized pain processes, or visualize an entrapment with a skilled practitioner.
The medications can help. Topical agents are a great option for this nerve specifically due to the relatively superficial nature of it.
Conventional RFA or pulsed RF are options. The peripheral nervous system does regenerate after a lesion, but my problem is that it isn't always perfect regeneration. In post-traumatic/surgical states where nerve trauma appears to have incited a pain state, my preference is to not cause more trauma with thermal ablation, although that's purely a theoretical concern as we do it all the time for facet joints, and this is a purely a sensory nerve we would be considering ablating. I prefer pulsed along with a nerve block as my first round of treatment, followed by PNS if needed/indicated before a conventional RFA.
The SPRINT system reportedly has long term benefits of over 12 months despite just 60 days of treatment. There are more durable implants out there if needed, both peripherally and at the level of the spinal cord/DRG.
A localized injection with ultrasound guidance can help delineate peripheral from centralized pain processes, or visualize an entrapment with a skilled practitioner.
- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,639
It may eventually get better on its own. In the meantime you can try a progression of treatments to see what works for you - nerve block with steroid, pulsed RF if that doesn’t last long enough, then thermal RF if that doesn’t.
I have one of these compound neuropathic creams, but doesn't seem to do much. Capsaicin cream seems to work better for me, but the strongest formulation is 0.1% and it wears off quickly, and the Qutenza patch didn't work for some reason. It does seem to be getting better in that I used to only be able to walk a pathetic 1500 steps a day in the spring, now I can walk about 3000 steps a day, with a crutch. Still pathetic but gradual activity progression has been working, painfully slowly.
- Joined
- Dec 13, 2005
- Messages
- 5,316
- Reaction score
- 3,596
That is pretty poor function. I would do another course of intensive PT with the best person in your town.
- Joined
- Dec 13, 2005
- Messages
- 5,316
- Reaction score
- 3,596
3000 steps and still using a crutch 10 months after a knee scope is terrible. I would change the whole crew helping you. Ortho 2nd opinion, pt 2nd opinion
- Joined
- Apr 13, 2016
- Messages
- 2,663
- Reaction score
- 2,639
Can you describe your symptoms a little more? We might be able to give you a better sense of options. The degree of pain and disability sounds like CRPS. What is the distribution of pain? Is it purely sensory or any weakness separate from the pain? Color/temperature changes?
I don't think it's CRPS, no temperature or colour changes. And it's not a burning type pain really. It's a soreness/fullness/ sometimes kinda buzzing but not like a paresthesia, sometimes kinda throbbing, that starts medial and inferopatellar right where the portal scar is, and radiates laterally. Worse with movements and knee bending. There is no weakness. Physio has been challenging because even 1 SLR can set it off into a flair. Has felt better this week though, since I started duloxetine I think.
- Joined
- Apr 6, 2013
- Messages
- 847
- Reaction score
- 415
Severe pain with SLR...lumbar MRI?
Also that is not consistent with a neuropathy to one of the tiny superficial nerves near the skin...
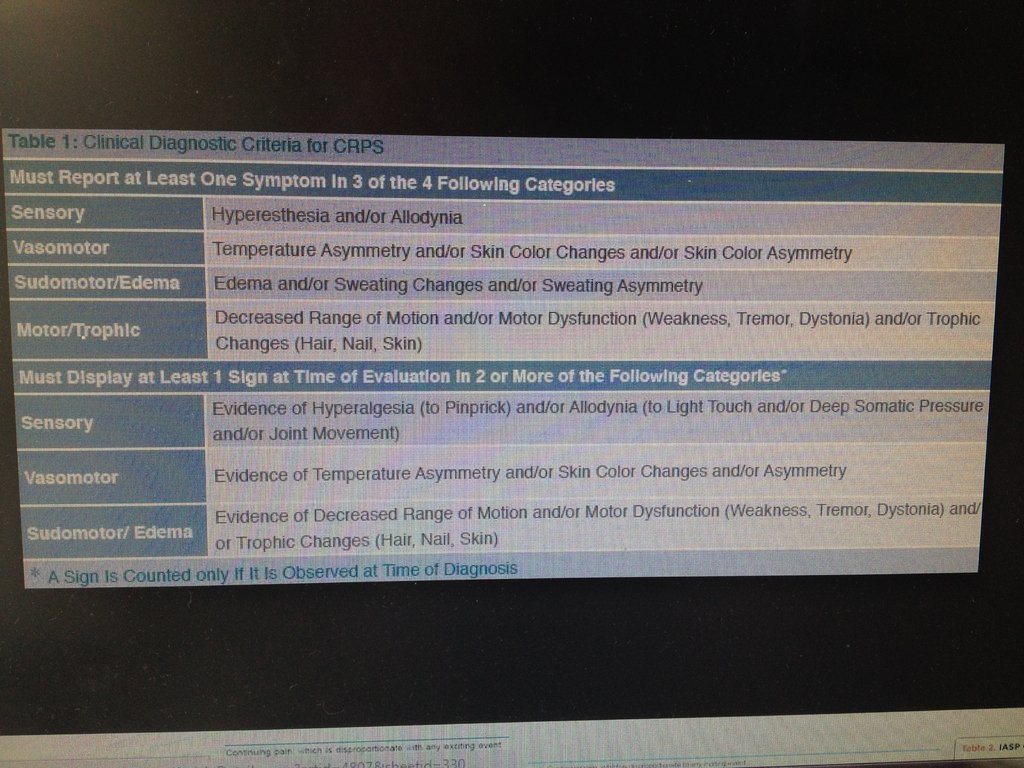
If u have decreased ROM and edema u you could meet the Budapest diagnostic criteria for CRPS
Pulsed RF has little downside but not a lot of great evidence, which is why insurances don’t pay
If I were u:
Increase cymbalta to 60 qHS
2nd ortho opinion to make sure there is nothing that is just mechanically messed up causing your issues
Ketamine gel
If 2nd opinion is non surgical...
Try PT with someone trained in CRPS
Desensitization protocols, mirror therapy, left right flash cards, graded motor imagery, etc
If all that fails, I would opt for the SPRINT system, because little downside and not very invasive or involving for you as the patient
Consider dorsal root ganglion stimulator if that fails
Sorry you have having such a rough go of it...hang in there.
Also that is not consistent with a neuropathy to one of the tiny superficial nerves near the skin...
If u have decreased ROM and edema u you could meet the Budapest diagnostic criteria for CRPS
Pulsed RF has little downside but not a lot of great evidence, which is why insurances don’t pay
If I were u:
Increase cymbalta to 60 qHS
2nd ortho opinion to make sure there is nothing that is just mechanically messed up causing your issues
Ketamine gel
If 2nd opinion is non surgical...
Try PT with someone trained in CRPS
Desensitization protocols, mirror therapy, left right flash cards, graded motor imagery, etc
If all that fails, I would opt for the SPRINT system, because little downside and not very invasive or involving for you as the patient
Consider dorsal root ganglion stimulator if that fails
Sorry you have having such a rough go of it...hang in there.
- Joined
- Oct 7, 2011
- Messages
- 14,655
- Reaction score
- 5,955
Not to be a spoilsport but we aren’t supposed to provide individual patient care on this forum.
I understand that you are a doctor but still...
I’d suggest that you PM the posters who have responded to your questions for personal and private information, or sit down with your pain doctor...
I understand that you are a doctor but still...
I’d suggest that you PM the posters who have responded to your questions for personal and private information, or sit down with your pain doctor...
- Joined
- Sep 28, 2015
- Messages
- 3,069
- Reaction score
- 3,778
Locking this, as it is against our TOS to seek medical advice (even if you are a provider).
- Status
- Not open for further replies.
Similar threads
- Replies
- 35
- Views
- 3K
