- Joined
- Jul 27, 2010
- Messages
- 1,813
- Reaction score
- 1,522
New study
 jamanetwork.com
jamanetwork.com
I am curious about the reliability of the diagnoses in the records review (e.g., misdiagnoses) and the overall covariance of general poor health in individuals with psychotic disorders but I thought an interesting finding.
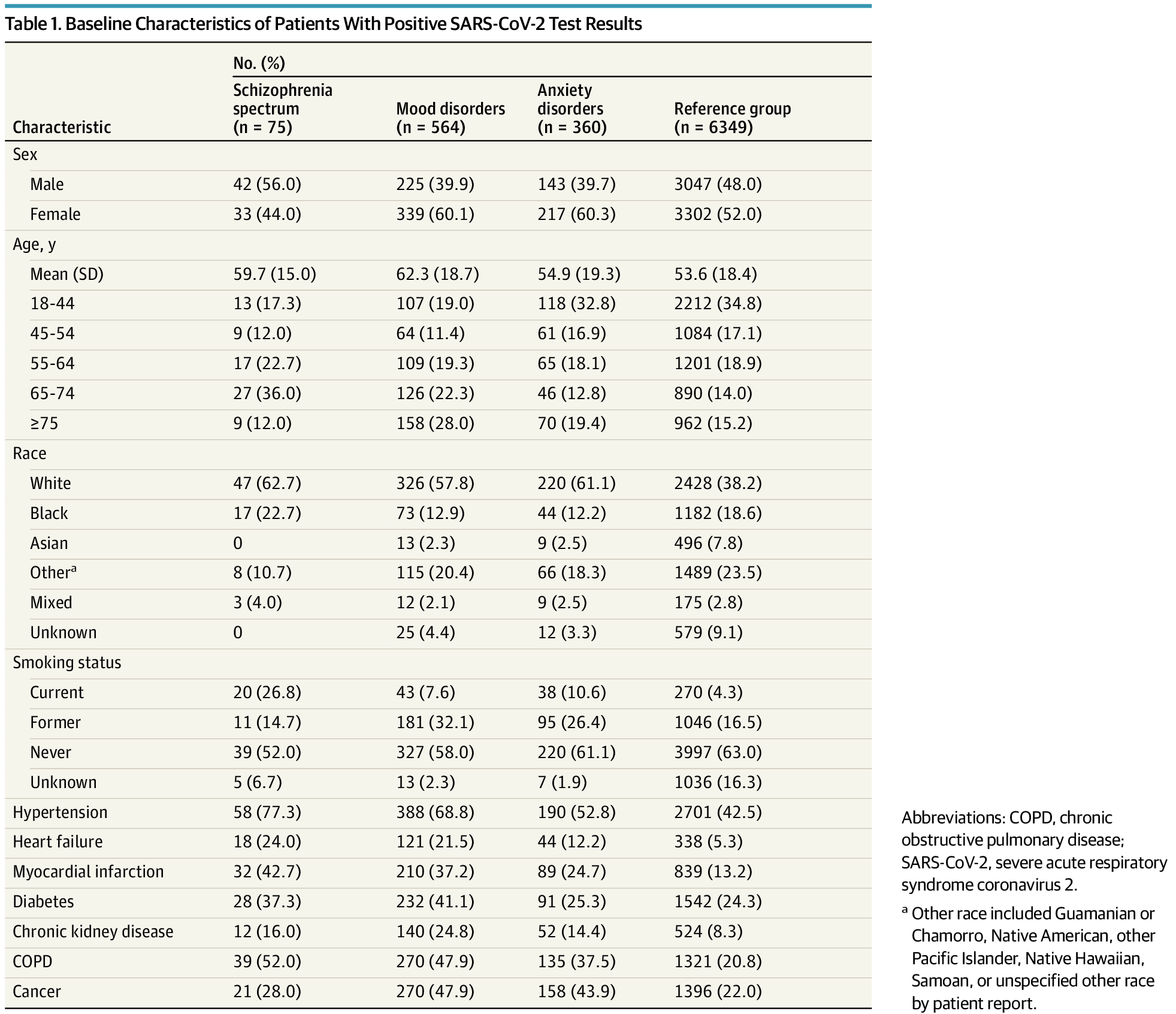
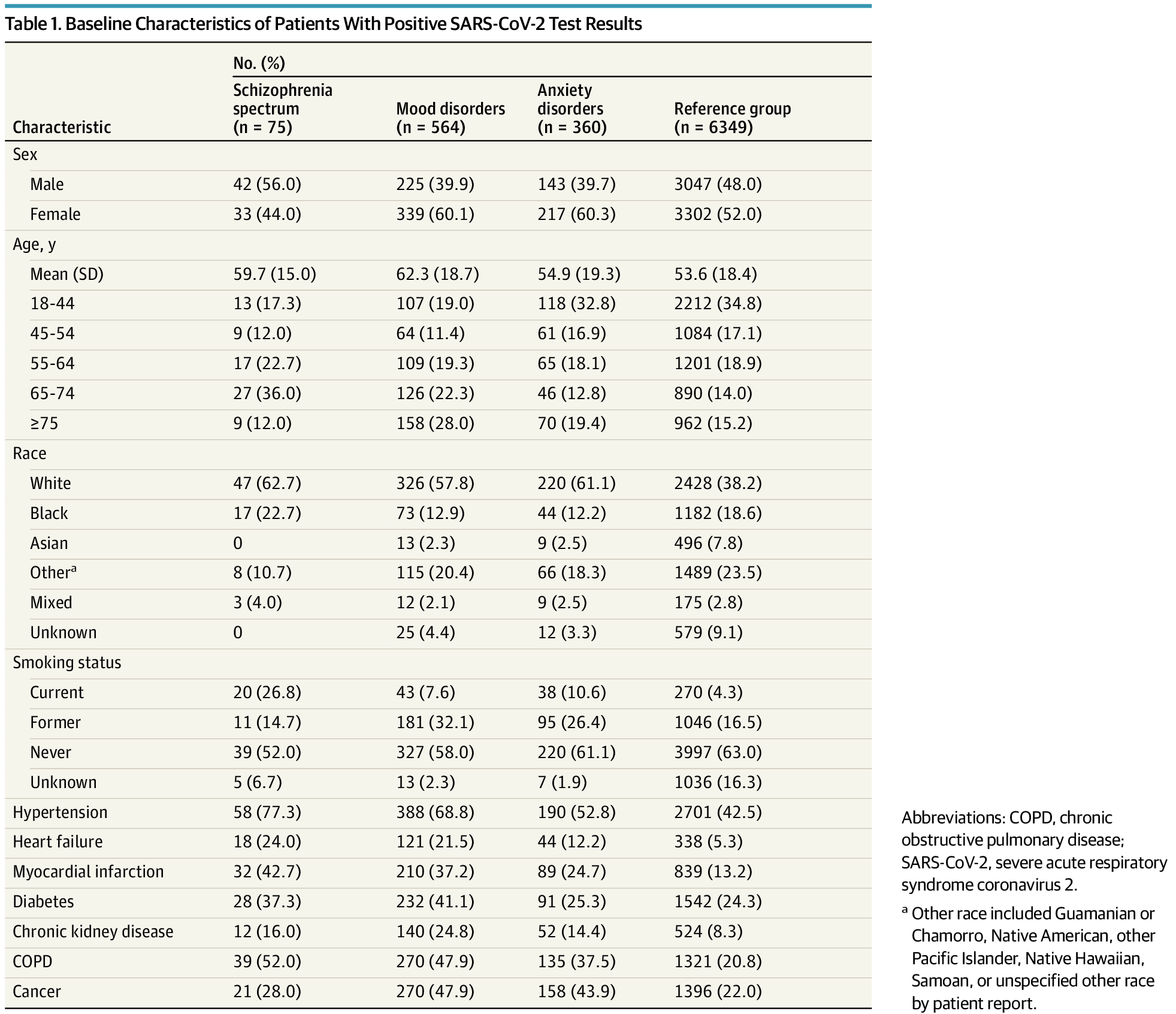
Association of Psychiatric Disorders With Mortality Among Patients With COVID-19
This cohort study examines the incidence of mortality in patients with COVID-19 who had premorbid diagnoses of schizophrenia spectrum, mood, or anxiety diagnoses.
In this cohort study of adults with SARS-CoV-2–positive test results in a large New York medical system, adults with a schizophrenia spectrum disorder diagnosis were associated with an increased risk for mortality, but those with mood and anxiety disorders were not associated with a risk of mortality.
I am curious about the reliability of the diagnoses in the records review (e.g., misdiagnoses) and the overall covariance of general poor health in individuals with psychotic disorders but I thought an interesting finding.
