- Joined
- May 7, 2020
- Messages
- 358
- Reaction score
- 70
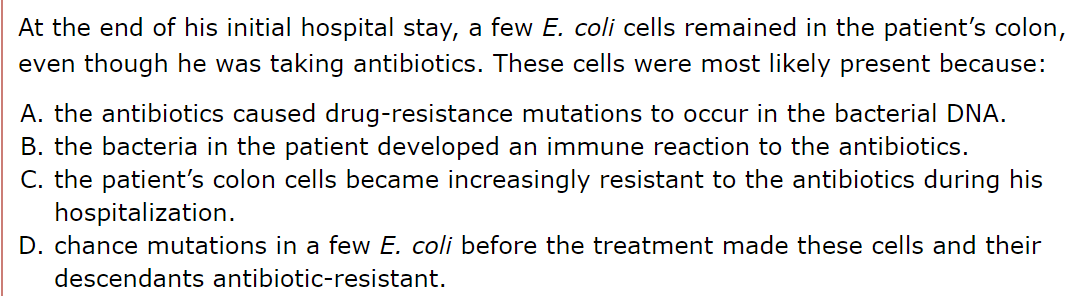
There was a question in the AAMC bio q pack 2, number 12: How is A not correct? The explanation states that "Antibiotics are unlikely to have been the source of the mutations"
What? I thought the whole idea behind superbugs, and antibiotic resistance problems in hospitals was that bacteria are able to mutate and become resistant to antibiotics. How is this incorrect?
I was stuck between A and D because they both seemed likely. Is antibiotic resistance as developed through mechanisms suggested by A something that takes a long period of time to happen? And thus why A might not be a good answer? His initial stay in the hospital was a few weeks.

 en.wikipedia.org
en.wikipedia.org
What? I thought the whole idea behind superbugs, and antibiotic resistance problems in hospitals was that bacteria are able to mutate and become resistant to antibiotics. How is this incorrect?
I was stuck between A and D because they both seemed likely. Is antibiotic resistance as developed through mechanisms suggested by A something that takes a long period of time to happen? And thus why A might not be a good answer? His initial stay in the hospital was a few weeks.

Antimicrobial resistance - Wikipedia
Last edited:
