- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
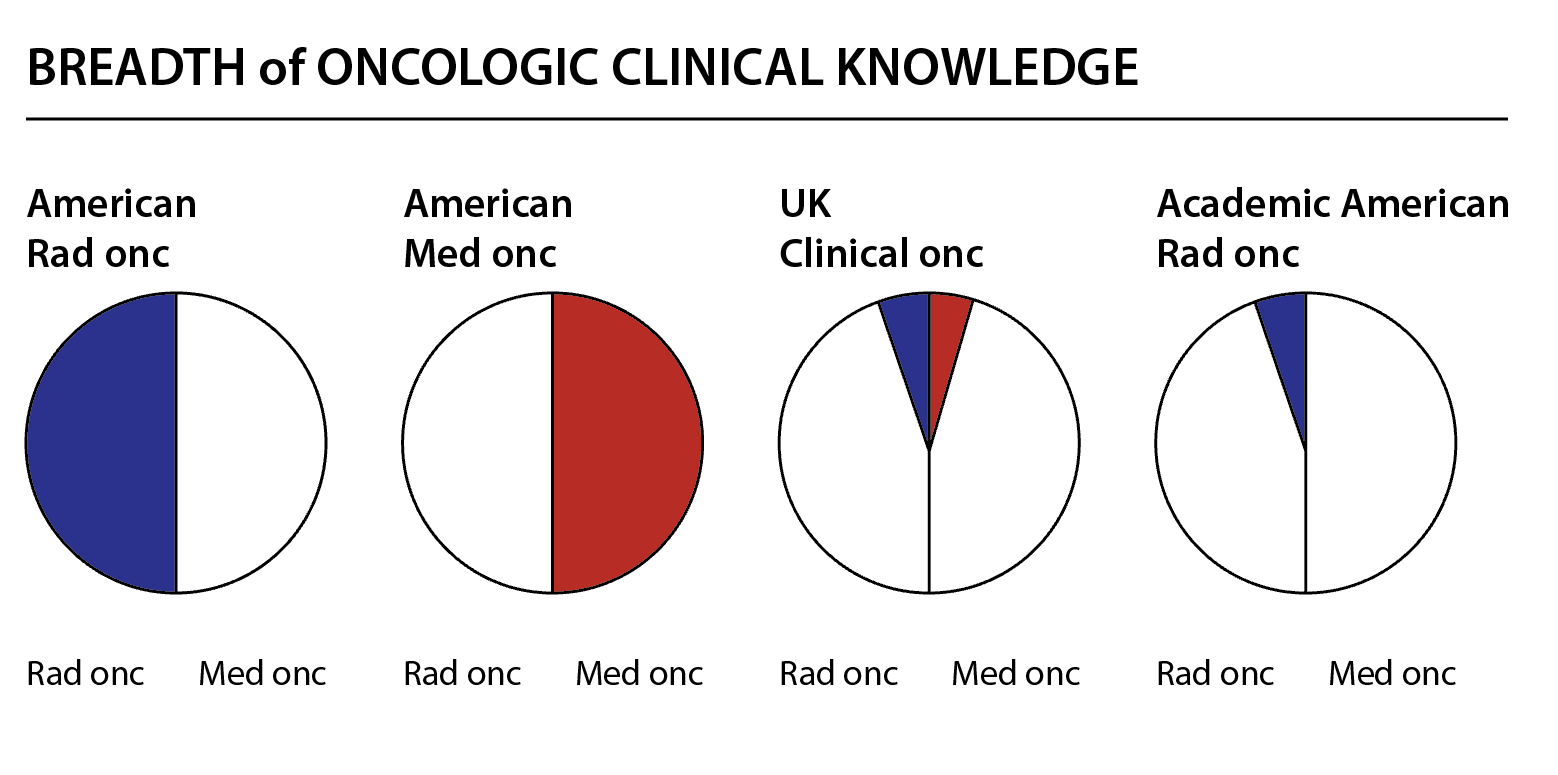
I believe we have covered this before and if so apologies in advance but I today had a mini-epiphany that there are no radiation oncologists in the UK. There are only medical oncologists (those who do non-surgical, non-RT cancer care) and clinical oncologists (those who do non-surgical cancer care). How interesting the huge difference in radiation medicine training in the US vs the UK. (Am pretty sure that there are radiation oncologists in Australia FWIW as a contradistinction.) That there would be a systemic-therapy and radiation-therapy-trained human makes more sense to me than sidling up to radiology, although either one sort of hints at the fact that a pure rad onc may be too one-trick-ponyish at least as we hurtle into the future. The revelation occurred to me because someone in the UK looked at physician job satisfaction and 1) reports that clinical oncologists ("medical oncologists who do radiation," in American parlance) are happier than medical oncologists, and 2) unsurprisingly, clinical oncologists have bigger workloads. If one truly wants to be an oncological polymath, UK clinical oncology training might be the way to go.