- Joined
- Jan 18, 2013
- Messages
- 152
- Reaction score
- 15
Dear colleagues,
I need your advice.
67 yo female, with metastatic breast cancer history to the bone, brain and lung.
Her disease was stable with second line treatment: Bone lesions symptomatic and stable, regression of lung lesions, with single ring enhanced secondary lesion of the right poster-lateral aspects of the pons at the level of the right middle cerebellar peduncle (1.4cm, PTV 1,6cc).
she received single fraction SRS 15Gy marginal dose in august 2020.
she tolerated very well with very good response till February 2021, when she presented with complete right peripheral facial palsy. Brain MRI showed progression of the same BS lesion with peri-lesional edema, as well as too new mm cerebellar lesions. Pet CT showed progression of the bony lesions, stable lung lesions.
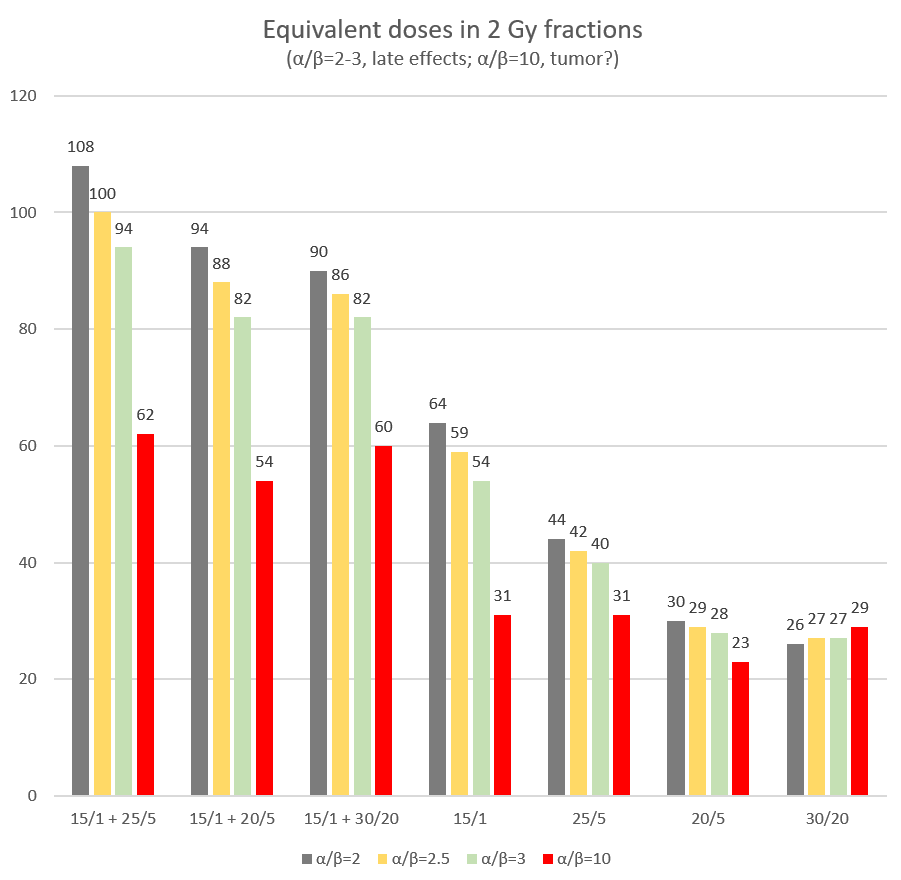
My plan is to give her Whole Brain with HS, SIB to the BS and cerebellar lesions, since she is progressing outside the brain too with no proof of potential effective third line treatment.
But what dose to give as re_rt to the BS lesion almost 7 month after first SRS?
I need your advice.
67 yo female, with metastatic breast cancer history to the bone, brain and lung.
Her disease was stable with second line treatment: Bone lesions symptomatic and stable, regression of lung lesions, with single ring enhanced secondary lesion of the right poster-lateral aspects of the pons at the level of the right middle cerebellar peduncle (1.4cm, PTV 1,6cc).
she received single fraction SRS 15Gy marginal dose in august 2020.
she tolerated very well with very good response till February 2021, when she presented with complete right peripheral facial palsy. Brain MRI showed progression of the same BS lesion with peri-lesional edema, as well as too new mm cerebellar lesions. Pet CT showed progression of the bony lesions, stable lung lesions.
My plan is to give her Whole Brain with HS, SIB to the BS and cerebellar lesions, since she is progressing outside the brain too with no proof of potential effective third line treatment.
But what dose to give as re_rt to the BS lesion almost 7 month after first SRS?
Attachments
Last edited: