At tumor board today, 65 yo man with T3N1 rectal cancer.
Low-lying tumor encroaching on the sphincter.
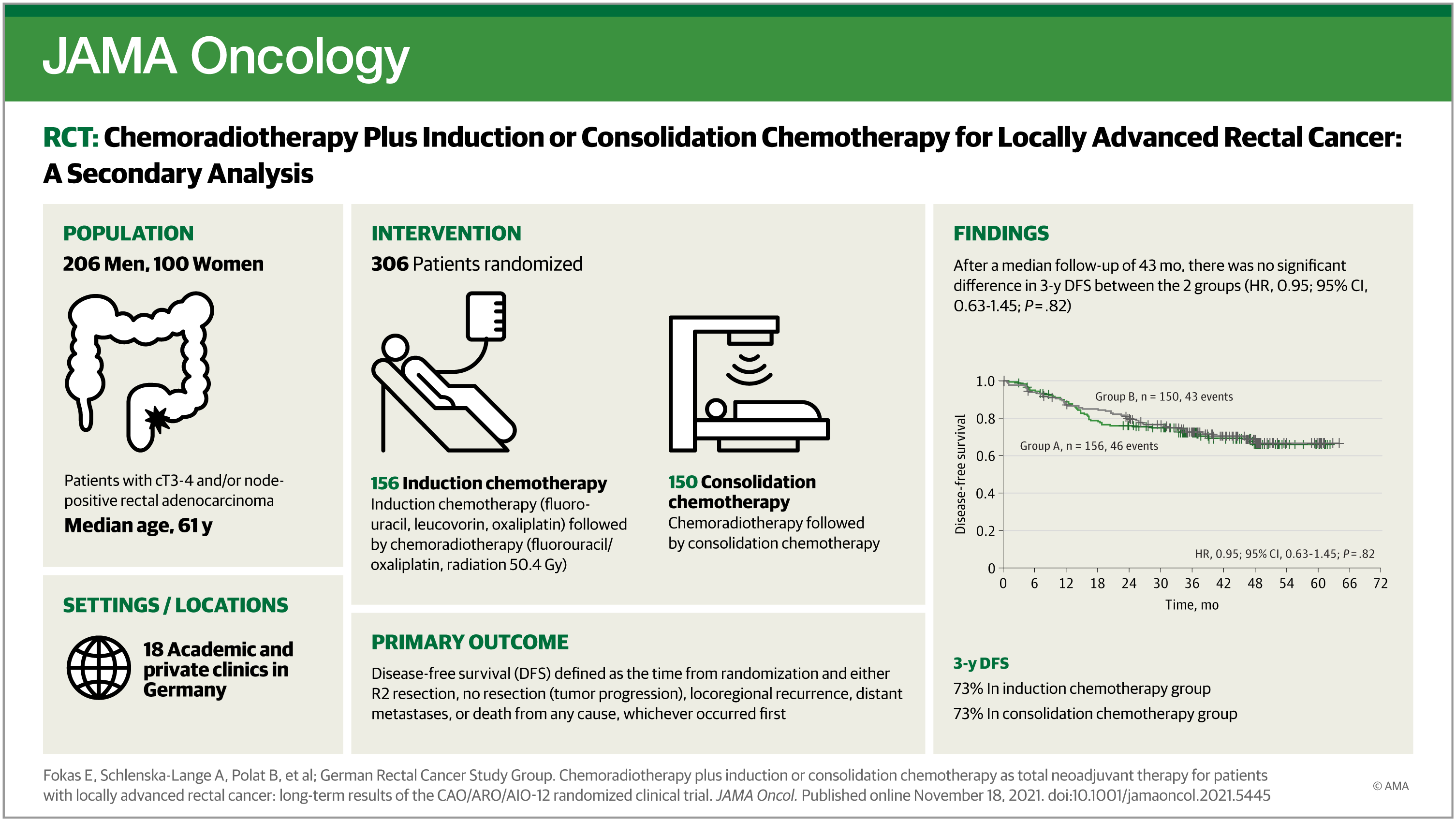
Colorectal surgeon argues for 1) ChemoRT ---> Chemo ---> Surg.
I am used to 2) Chemo ---> ChemoRT (wait 6-8 wks) ---> Surg.
The CR surgeons claim that Annals of Surgery article says #1 is better bc of higher pCR in that cohort "about 11% more pCR in approach #1"...blah blah blah.
They pointed me to this article in Annals of Surg (BTW, primary author is a colorectal surg fellow, no radonc
authors in the paper, and this is the usual "infamous" NCDB study).
Primary author is Goffredo, Paolo et al (Division of Colon & Rectal Surgery, Department of Surgery, University of Minnesota, Minneapolis, MN)...
 journals.lww.com
journals.lww.com
I have never done #1 bc of long interval between RT and Surg and risks of increased fibrosis.
I do not have access to Annals of Surg.
Does anyone know the pros and cons (any data on the observation study) for approach #1?
Thanks...
PS: Maybe the surgeons quoted the wrong paper but he mentioned Annals of Surg a few months ago.
Low-lying tumor encroaching on the sphincter.
Colorectal surgeon argues for 1) ChemoRT ---> Chemo ---> Surg.
I am used to 2) Chemo ---> ChemoRT (wait 6-8 wks) ---> Surg.
The CR surgeons claim that Annals of Surgery article says #1 is better bc of higher pCR in that cohort "about 11% more pCR in approach #1"...blah blah blah.
They pointed me to this article in Annals of Surg (BTW, primary author is a colorectal surg fellow, no radonc
authors in the paper, and this is the usual "infamous" NCDB study).
Primary author is Goffredo, Paolo et al (Division of Colon & Rectal Surgery, Department of Surgery, University of Minnesota, Minneapolis, MN)...
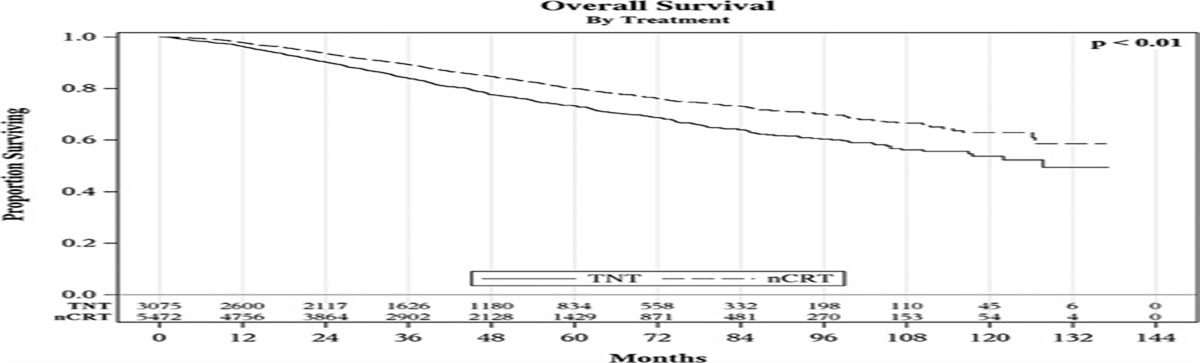
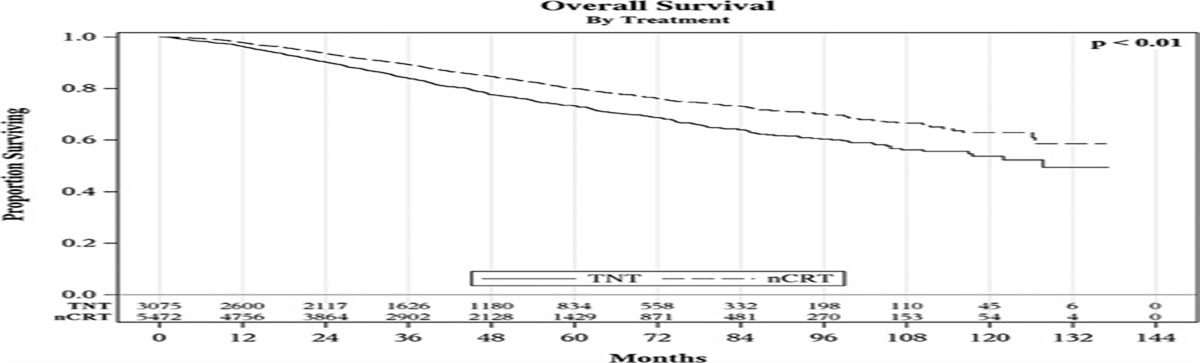
Total Neoadjuvant Therapy Versus Standard Neoadjuvant... : Annals of Surgery
nts with locally advanced rectal cancer. Summary of Background Data: Outside of clinical trials and small institutional reports, there is a paucity of data regarding the short and long-term oncologic impact of TNT as compared to nCRT. Methods: Adult patients with stage II-III rectal...
I have never done #1 bc of long interval between RT and Surg and risks of increased fibrosis.
I do not have access to Annals of Surg.
Does anyone know the pros and cons (any data on the observation study) for approach #1?
Thanks...
PS: Maybe the surgeons quoted the wrong paper but he mentioned Annals of Surg a few months ago.