- Joined
- Jun 2, 2008
- Messages
- 14
- Reaction score
- 0
did not see it addressed in any other thread, so...
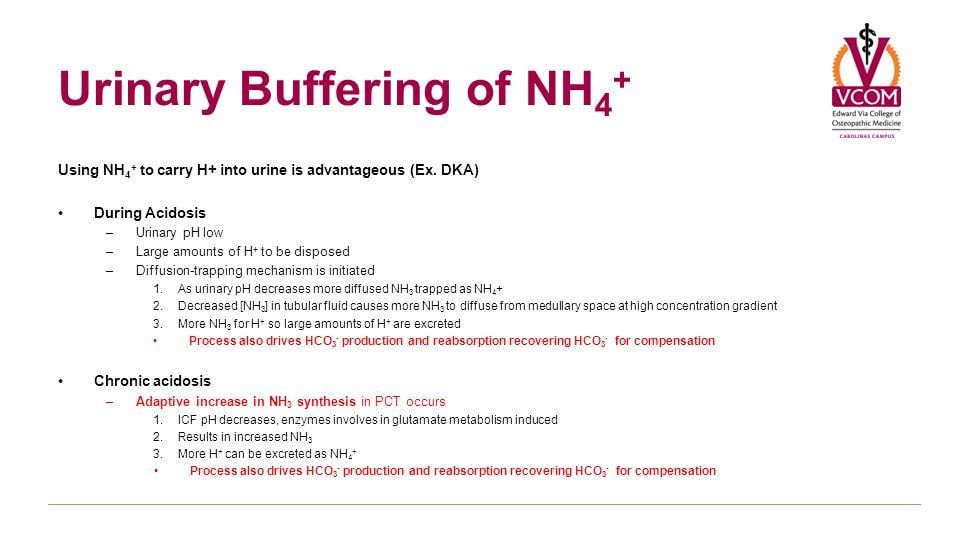
can someone explain to me why hypoaldosteronism ---> (hyperkalemia) --> decreased secretion of ammonia(ium). I don't understand the mechanism of decreased NH3 excretion, so I will never be able to "learn" it. Hopefully it's easy, but does not seem to be addressed by books I have.
thanks fellas and ladies.
can someone explain to me why hypoaldosteronism ---> (hyperkalemia) --> decreased secretion of ammonia(ium). I don't understand the mechanism of decreased NH3 excretion, so I will never be able to "learn" it. Hopefully it's easy, but does not seem to be addressed by books I have.
thanks fellas and ladies.