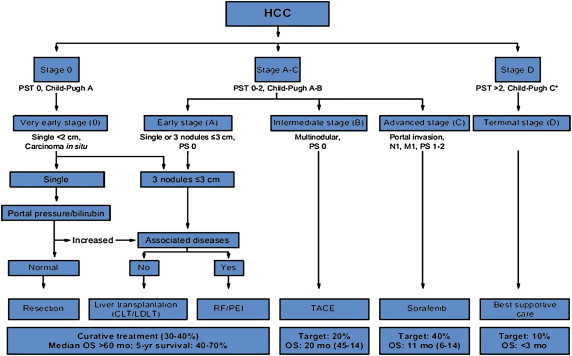
Anyone have any insight into how and when to make recommendations for SRS liver at tumor board. Somewhat frequently a patient is presented with HCC or 1-3 oligometastasis to liver and is unresectable or needs a bridge to transplant. I often think I could easily meet dose constraints and provide local control but these people invariably get sent to IR for TACE. I have done some literature review and have brought up the following articles when appropriate with little enthusiasm from anyone at the tumor board.
https://www.ncbi.nlm.nih.gov/pubmed/23216217
http://www.advancesradonc.org/article/S2452-1094(15)00009-3/abstract?cc=y=
I was wondering if anyone has insight or evidence that could help me make a better argument for SRS liver or at least refine the patient population that a radiation oncologist should push hard for treating.
https://www.ncbi.nlm.nih.gov/pubmed/23216217
http://www.advancesradonc.org/article/S2452-1094(15)00009-3/abstract?cc=y=
I was wondering if anyone has insight or evidence that could help me make a better argument for SRS liver or at least refine the patient population that a radiation oncologist should push hard for treating.