- Joined
- Jun 16, 2009
- Messages
- 204
- Reaction score
- 185
So United Health Group has decided they are just going to ignore the CMS RUC physician payment schedule and downcode all Level 5 charts it deems unworthy. Per article, United " Optum Evaluation and Management Professional (E&M Pro) tool will determine the “correct” code-based solely on the patient’s age and the diagnoses submitted on the claim – and if the tool determines that the submitted diagnoses justify a lower-level code, the claim will either be automatically adjusted to the lower-level code or denied “based on the reimbursement structure” in their contract."
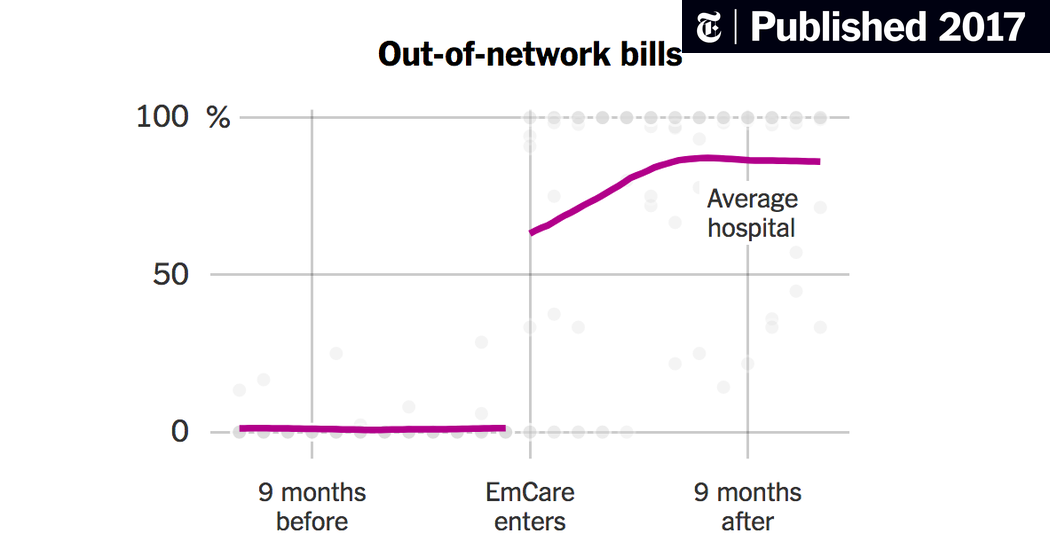
This is a huge hit to all EM, given we get 70-80% of our revenue from commercial contracts and UHG is largest insurer in US. In response, Team Health is passing on its hit directly to its doctors, including cutting pay and services like scribes. While I'm sure a lot of us feel schadenfreude for the CMG's, this will eventually pass on to every group. Times are looking bad--this, combined with benchmark fight by insurers, recent headlines of doctors making too much...the war is on doctors, EMTALA ones in particular. Add to this UHG Optum buying up doctor groups, NP's fighting for expansion everywhere...
Everyone here needs to get involved, and MS's, Residents, you guys need to educate yourselves on the current environment of EM. Academics need to stop sitting on their hands and start speaking up for EM everywhere while lobbyists, journalists, and economists rip us up. I fear we've hit the highwater mark of EM--Reimbursement seen 5-10 years ago won't be seen again.
This is a huge hit to all EM, given we get 70-80% of our revenue from commercial contracts and UHG is largest insurer in US. In response, Team Health is passing on its hit directly to its doctors, including cutting pay and services like scribes. While I'm sure a lot of us feel schadenfreude for the CMG's, this will eventually pass on to every group. Times are looking bad--this, combined with benchmark fight by insurers, recent headlines of doctors making too much...the war is on doctors, EMTALA ones in particular. Add to this UHG Optum buying up doctor groups, NP's fighting for expansion everywhere...
Everyone here needs to get involved, and MS's, Residents, you guys need to educate yourselves on the current environment of EM. Academics need to stop sitting on their hands and start speaking up for EM everywhere while lobbyists, journalists, and economists rip us up. I fear we've hit the highwater mark of EM--Reimbursement seen 5-10 years ago won't be seen again.