- Joined
- Jun 16, 2009
- Messages
- 204
- Reaction score
- 185
Their operating expenses were more than $220B last year. Their net and operating margins for the past few years seem fluctuate between 4-10% - similar to just about every other well-run insurance company.
Are you equally offended to know that your telecom provider probably brought in similar profit and operates at more than double those margins? Or, is the frustration limited to the businesses that more directly impact your bottom line?
You do realize 14 B (it was actually 19 B in EBITDA in 2019) is the 19th most profitable company in the world, more than Microsoft, Disney, or Toyota). UHG pulls in more profit than Blackstone (TH owner) or KKR (Envision) make. Poor $750 B insurance companies. The big reason doctors are in the situation they are in is b/c they are naive about how business and politics work. Health Insurers commit billions in fraud a year, and people here are quoting insurer-funded studies blaming doctors.
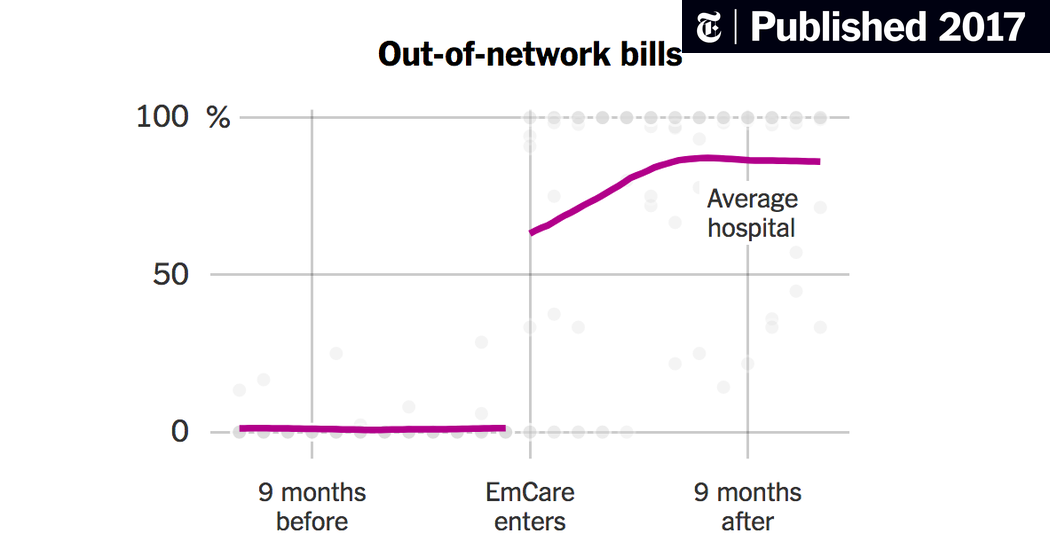
Truth of the matter is that average ED collection per bill is about $150 or so, which is less than it costs to get a plumber to your house. EMTALA is an unfunded mandate that shift costs to commercial payors, who have decided they don't want to pay any more. Yes their profit margins are relatively modest at 5%, but their revenue has increased 10% per year (United has 245B in revenue), which equals what they've raised in premiums and deductibles every year. Add to this fact they now own PBM's, which lets them skirt the MLR. Optum also bought Davita, making it the largest employer of physicians in the country.
Truth is pay is coming down, and politicians and insurers are scrambling to find cheaper care. That means NP's will be "just as good as doctors" and capitation will be the norm. It's up to doctors to defend what they do, and in EM, every patient gets subsequently more complex every year due to co-morbidities, aging population, and lack of decent primary care follow-up. EM has one of hardest job out there--we need to take ownership over what we do, stop letting suits buy the groups which maximize profit by cutting staffing and squeezing every drop out of the charts, and come up with new, innovative ways to provide better healthcare to patients when they get discharged. It's up to us to educate ourselves on business management and govt. policy, and come up with solutions. Stop listening to the media, politicians, and talking economists who couldn't even run a McDonalds who are trying to tell us how to manage patients.
Otherwise, we're toast.