A few things to keep in mind:
For much of CPT no single specialty holds a monopoly on the delivery of any given code. Sure, orthopods do most (if not all) of the joint replacements, neurosurg WTF ever it is they do, and derm provides the bulk of the micrographic surgery -- but we all provide E&M. Many specialties provide skin biopsies, local destructions, excisions, etc. It has to be appreciated that changes will not always have their desired effects; for example, boosting E&M reimbursement will have a more significant impact for high volume specialties (such as derm) more so than it will for specialties who deal with more complex / complicated / or intensive patients. Decreases in the RVU value for biopsies, excisions, local destructions, etc will have a greater impact on derm, but they will also have an impact on any specialty who provides those services. Bottom line is that income redistribution within medicine is not as simple and straightforward as some of our more simple and straightforward individuals proclaim.
on edit -- the reason that the above is important is the way the RUC works; codes undergo periodic (generally 5yr reviews, shorter time periods if CMS believes they are "overvalued" and thus driving too much utilization). Since many specialties provide some codes, the practice expense and physician work components will not always be equitable between specialties or providers. It may well be that it costs more for a PCP to perform a biopsy, destruction, or level 3 E&M than it does the dermatologist because the dermatologist has efficiencies of scale and a larger revenue/hr backdrop -- or vice versa if the dermatologist has a higher overhead/hr than the PCP, etc.... something that would be exceedingly difficult to factor in or otherwise account for within the confines of the RUC system.
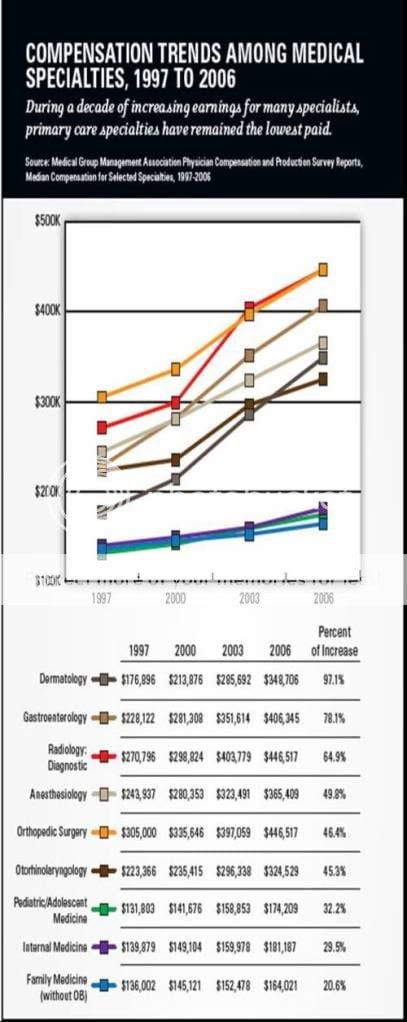
It is equally important to realize that a ton of variables factor into the median income figure... and while CPT mix is a major component, it is by no means the only one. Workforce demographics, practice arrangements, and the income distribution within any given specialty varies significantly. For example, dermatology has amongst the highest percentage of solo practitioners for any specialty; we also have a very high single specialty percentage. These things, taken together, have the net effect of skewing the median higher for any given level of revenue; if we had a higher MSG mix our numbers would invariably be lower. If you have any reason to doubt this, one of the more useful sets of data reported by the MGMA is the compensation per RVU for different practice settings by specialty.
Lastly, there is no great single metric for determining the "fairness" of compensation because there is no way to control for these myriad of variables. If we are to go on median incomes alone we would at least have to study the distribution of income, RVUs produced, total revenues, and compensation per RVU within each repspective specialty... We must continue to reward productivity and efficiency in some way as people should be paid for the amount of quality services they provide. The real problem is in the valuation of the units of service... which is what the RVU system was designed to address. It's not perfect, that's for sure, but I have not heard a better plan to date (other than forgoing the whole CPT system and direct billing patients for the service provided, which is a pipe dream today for most).