- Joined
- Apr 5, 2012
- Messages
- 1,667
- Reaction score
- 1,430
Hello.
I am a part time nephrologist / Internist who sees a large number of hypertensive and diabetic patients.
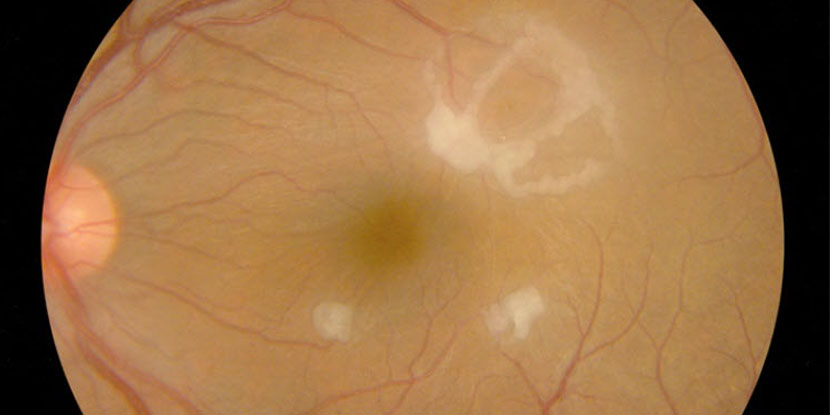
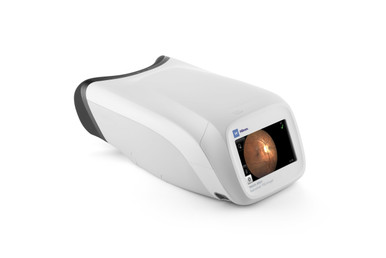
Although I do send these patients to opthalmology for a formal dilated retinal exam (which is part of the diabetes management anyway), I do have a PanOptic ophthalmoscope which I fiddle around with now and then for someone who is having uncontrolled BP for an undilated exam. It's not where near as good as those retinal photographs in the textbooks, of course. But I have gleaned some useful information in the past such as papilledema, A-V nicking, copper wiring, hard exudate etc...
I use the iphone attachment and Welch Allyn app to record and then pull stills for the record.
Personally, this has never changed my management yet... though I am still waiting for that one case of identifying malignant hypertension versus alternate etiologies of thrombotic microangiography in which the papilledema helps distinguish the etiologies... I may as well wait for Godot...
But I have heard all the arguments from all sides in the academic sphere.
Medical school educators and some old school Internists, Neurologists, and Nephrologists are state that the Internist should be able to see the fundus and glean the basic information. They all lament the "loss of the physical examination."
On the other hand, some of the same physicians express some degree of nihilism with statements such as:
- You can't see anything with a direct funduscope that is undilated anyway (counter - use the Panoptic)
- An internist without the proper medical malpractice insurance should not be dilating the eyes and triggering closed angle glaucoma (I have also heard the opthalmologist counter that if that happens, one is doing the patient a favor by identifying the issue... assuming an opthalmologist is ready and willing to come to assist and not grumble about "why'd you do that?")
- Even if you see papilledema you are already treating the hypertension based on other clinical metrics and already getting a CT head or other neuroimaging
- You need the full exam with an indirect scope or retinal photograph by the opthalmologist anyway to complete the chart and protect against a lawsuit.
What is the opthalmologist's take on this?
I would venture a guess and say "cool if you can see something but you should always refer if you are concerned."
(and then the PGY2 optho resident grumbles as he/she has to bring the luggage case to the wards)
My personal take is... it might help me convince someone in the outpatient setting to start BP meds if he/she is unconvinced by the other lab / imaging/ or clinical metrics... maybe...
I am a part time nephrologist / Internist who sees a large number of hypertensive and diabetic patients.
Although I do send these patients to opthalmology for a formal dilated retinal exam (which is part of the diabetes management anyway), I do have a PanOptic ophthalmoscope which I fiddle around with now and then for someone who is having uncontrolled BP for an undilated exam. It's not where near as good as those retinal photographs in the textbooks, of course. But I have gleaned some useful information in the past such as papilledema, A-V nicking, copper wiring, hard exudate etc...
I use the iphone attachment and Welch Allyn app to record and then pull stills for the record.
Personally, this has never changed my management yet... though I am still waiting for that one case of identifying malignant hypertension versus alternate etiologies of thrombotic microangiography in which the papilledema helps distinguish the etiologies... I may as well wait for Godot...
But I have heard all the arguments from all sides in the academic sphere.
Medical school educators and some old school Internists, Neurologists, and Nephrologists are state that the Internist should be able to see the fundus and glean the basic information. They all lament the "loss of the physical examination."
On the other hand, some of the same physicians express some degree of nihilism with statements such as:
- You can't see anything with a direct funduscope that is undilated anyway (counter - use the Panoptic)
- An internist without the proper medical malpractice insurance should not be dilating the eyes and triggering closed angle glaucoma (I have also heard the opthalmologist counter that if that happens, one is doing the patient a favor by identifying the issue... assuming an opthalmologist is ready and willing to come to assist and not grumble about "why'd you do that?")
- Even if you see papilledema you are already treating the hypertension based on other clinical metrics and already getting a CT head or other neuroimaging
- You need the full exam with an indirect scope or retinal photograph by the opthalmologist anyway to complete the chart and protect against a lawsuit.
What is the opthalmologist's take on this?
I would venture a guess and say "cool if you can see something but you should always refer if you are concerned."
(and then the PGY2 optho resident grumbles as he/she has to bring the luggage case to the wards)
My personal take is... it might help me convince someone in the outpatient setting to start BP meds if he/she is unconvinced by the other lab / imaging/ or clinical metrics... maybe...