- Joined
- Jan 12, 2006
- Messages
- 143
- Reaction score
- 5
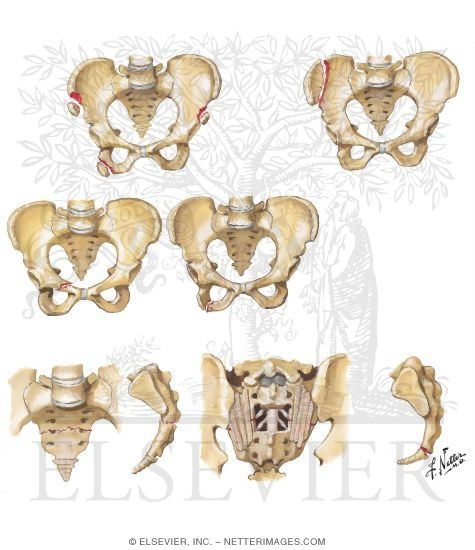
17 yo female with no prev PHMx involved in MVA with ejection, large pelvic ring fracture, spleen is bleeding with bowel bleeding as well. She comes to the OR on face mask with blood running through the level 1.
Hb downstairs is 3.7 after 2 Units PRBC given. Good start to case with large bore IV's and art line placed. Belmont infuser is cranking with med student alternating FFP/PRBC while I and others manage hypotension with phenylephrine and norepi.
After about 1 hour, I noticed capnograph not reading and it reading occlusion. I looked up to see fluid refluxing back into the Dfend spirometry sensor. Next looked down at ETT to see fluid pouring up out the tube. Horrible pulmonary edema
We had to disconnect her from the circuit and just let it pour out of the tube like 15 times in the next 30 mins. Gave morphine once and lasix 20mg x 4. Manually ventilated her for the next 20 min.
She eventually got 22 Units PRBC, 14 FFP, 3 Units platelets, and 1 cellsaver bag. She was continually bleeding the entire time and they were not sure that all of her pelvic bleeding had stopped. Procedures ended up being a splenectomy, bowel resection, and pelvic ex-fix and also some repair on the perineum for open lacs. I am a CA-2 and have only seen this pulmonary edema once in an old CHF lady just after intubation in the ICU.
Any other experiences/suggestions for management? Too much product given? She was pretty dependent on the products infusing to maintain her BP. We evenutally got her packed up and ran to the ICU, she acutally had stabilized slightly when we got to the ICU
Hb downstairs is 3.7 after 2 Units PRBC given. Good start to case with large bore IV's and art line placed. Belmont infuser is cranking with med student alternating FFP/PRBC while I and others manage hypotension with phenylephrine and norepi.
After about 1 hour, I noticed capnograph not reading and it reading occlusion. I looked up to see fluid refluxing back into the Dfend spirometry sensor. Next looked down at ETT to see fluid pouring up out the tube. Horrible pulmonary edema
We had to disconnect her from the circuit and just let it pour out of the tube like 15 times in the next 30 mins. Gave morphine once and lasix 20mg x 4. Manually ventilated her for the next 20 min.
She eventually got 22 Units PRBC, 14 FFP, 3 Units platelets, and 1 cellsaver bag. She was continually bleeding the entire time and they were not sure that all of her pelvic bleeding had stopped. Procedures ended up being a splenectomy, bowel resection, and pelvic ex-fix and also some repair on the perineum for open lacs. I am a CA-2 and have only seen this pulmonary edema once in an old CHF lady just after intubation in the ICU.
Any other experiences/suggestions for management? Too much product given? She was pretty dependent on the products infusing to maintain her BP. We evenutally got her packed up and ran to the ICU, she acutally had stabilized slightly when we got to the ICU